Maternal mortality in the U.S. remains a critical public health concern, as recent data highlights the alarming rise in pregnancy-related deaths. Despite being a high-income nation, the U.S. leads its peers with a maternal mortality rate that has not only persisted but escalated in recent years. A staggering 80% of these deaths are deemed preventable, spotlighting significant maternal health disparities across different states and demographics. The rise in cardiovascular disease as a leading concern during pregnancy further exacerbates these statistics, emphasizing the need for comprehensive prenatal and postpartum care. Addressing these issues is paramount to ensuring healthier outcomes for mothers and their newborns in an era marked by rising U.S. pregnancy statistics.
In recent years, the issue of maternal mortality in America’s healthcare landscape has gained urgent attention, with increasing instances of pregnancy-related fatalities. Terms like maternal death rates and health inequities are prevalent as researchers dissect the complex factors contributing to this troubling trend. Several recent studies indicate a correlation between cardiovascular conditions and pregnancy, leading to greater fatalities among expectant mothers. Furthermore, disparities in access to quality maternal health care reveal alarming patterns, particularly among marginalized communities. Thus, the emphasis on effective postpartum care becomes crucial in addressing the multifaceted challenges surrounding maternal health and reducing preventable fatalities.
The Alarming Increase in Maternal Mortality in the U.S.
The United States boasts the highest maternal mortality rate among high-income nations, and recent studies reveal that the situation is worsening. From 2018 to 2022, the maternal mortality rate saw a significant increase, with particularly sharp spikes noted during the COVID-19 pandemic. This alarming trend illustrates the urgent need for effective interventions to address preventable pregnancy-related deaths, as over 80% of these deaths are deemed preventable. The call for improved prenatal care and comprehensive postpartum support has never been more critical, as we strive to reduce this troubling statistic.
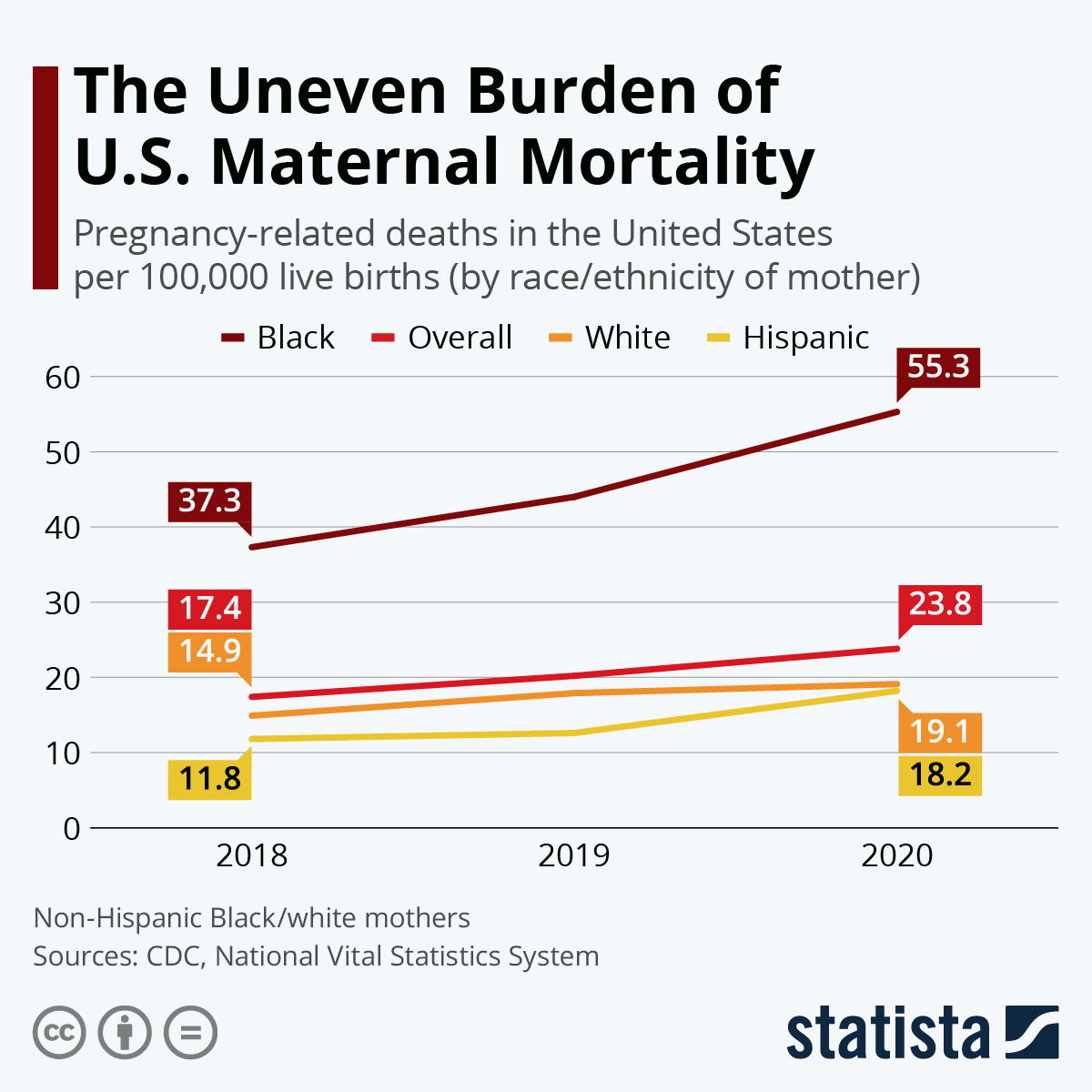
Disparities in maternal health further exacerbate the issue, with racial and ethnic minorities facing disproportionate challenges. For instance, American Indian and Alaska Native women experience mortality rates nearly four times higher than their white counterparts. These stark differences highlight the systemic flaws in the healthcare system that contribute to maternal mortality in the U.S. It is imperative that we work to rectify these disparities through targeted policies and initiatives that ensure equitable access to quality maternal healthcare.
Understanding Pregnancy-Related Deaths: Causes and Disparities
Pregnancy-related deaths can arise from various causes, with cardiovascular disease emerging as one of the leading threats to maternal health. This shift from historical causes, such as hemorrhage, to chronic conditions like hypertension and heart disease indicates a concerning trend of deteriorating maternal health among diverse demographics. Researchers have found that younger populations are now expressing these chronic conditions at alarming rates, posing significant risks during pregnancy.
Maternity care deserts and inequitable healthcare access further exacerbate the already significant maternal health disparities. Many individuals, especially from marginalized communities, find it challenging to access necessary prenatal care and postpartum resources. This leads to insufficient monitoring, delayed treatments, and ultimately higher mortality rates. Addressing these disparities is essential for fostering a maternal health environment where all women receive the care they deserve throughout the entire pregnancy continuum.
Postpartum Care Importance: A Continuous Journey
Postpartum care should be recognized as a critical phase for maternal health, extending beyond the conventional six-week checkup. Recent studies indicate that nearly a third of maternal deaths occur after the initial postpartum period, particularly emphasizing the need for ongoing healthcare after childbirth. By expanding the timeframe in which postpartum health is monitored, healthcare providers can intervene more effectively and prevent potential complications.
Investing in comprehensive postpartum care not only allows for better management of physical health but also addresses mental health challenges that many new mothers face. Improved support systems during this vulnerable time can significantly enhance long-term maternal and infant health outcomes. As more attention is given to the postpartum experience, the emphasis on creating a continuum of care for mothers becomes increasingly clear—setting a foundation for healthier families.
The Role of Cardiovascular Disease in Maternal Health
Cardiovascular disease is now recognized as a leading cause of pregnancy-related death in the United States, accounting for over 20% of fatalities. The increase in rates among younger women, particularly those in the 25 to 39 age range, underscores the necessity for proactive monitoring and management of chronic health issues before and during pregnancy. As chronic conditions like hypertension become prevalent in younger populations, it’s essential for healthcare providers to assess these risks early on.
Furthermore, the impact of cardiovascular health on pregnancy outcomes cannot be overstated. The transition to a more cardiovascular-focused approach in maternal health care is vital in reducing pregnancy-related mortality rates. By prioritizing education about heart health and creating targeted interventions for at-risk populations, healthcare systems can make considerable progress in safeguarding mothers’ lives.
Preventing Maternal Mortality: Policy Changes Needed
Amid rising maternal mortality rates, there is a pressing need for comprehensive policy changes to address the underlying issues affecting maternal health. The disparities highlighted in recent studies reveal that some states perform significantly better than others, indicating that state-level policies and healthcare practices play a pivotal role. Implementing effective interventions tailored to each state’s unique challenges can drastically alter the maternal health landscape in the U.S.
Beyond addressing state disparities, investing in public health infrastructure is crucial for tracking and improving maternal health outcomes. Without adequate data collection and analysis, as seen in the recent increase in maternal mortality rates, informed policy-making becomes virtually impossible. Advocacy for enhanced research funding and a focus on maternal health will ensure we take meaningful steps towards improving care for all birthing individuals.
The Impact of Racial Disparities in Maternal Health
Racial disparities in maternal mortality rates are profound, with marginalized communities facing far greater risks than their white counterparts. Studies show that American Indian and Alaska Native women experience mortality rates nearly four times higher than white women. These alarming statistics highlight the critical role systemic bias and healthcare inequities play in exacerbating the crisis in maternal health.
Addressing these disparities necessitates a multifaceted approach, including policy reform and enhanced training for healthcare professionals on implicit biases. By prioritizing culturally competent care and ensuring equitable access to resources, we can work towards a healthcare landscape that provides fair and just maternal health outcomes for all women, regardless of their racial or ethnic background.
The Importance of Comprehensive Maternal Health Research
A critical aspect of improving maternal health outcomes lies in ongoing research and data collection. Until recently, the United States lacked a reliable national system for tracking pregnancy-related deaths, making it difficult to identify patterns and develop effective interventions. With the establishment of a standardized pregnancy checkbox on death certificates, future research looks promising, yet continued investment and commitment are required to ensure quality data is collected and analyzed.
Moreover, research not only informs policy but also drives innovation in maternal healthcare practices. By understanding the complexities of maternal health challenges, including those rooted in socioeconomic factors or chronic conditions, researchers can develop targeted solutions that address unique populations’ needs. This commitment to understanding and managing maternal mortality through rigorous research is essential to achieving sustainable improvements.
Innovative Solutions to Combat Maternal Mortality
Innovative solutions must be employed to address the increasing rates of maternal mortality in the U.S. From improving access to telehealth services for prenatal and postpartum care to ensuring quality education for healthcare providers, creative strategies can significantly influence maternal health outcomes. By leveraging technology, far-reaching benefits can be realized in terms of accessibility, effectiveness of care, and patient engagement.
Additionally, community-based programs that focus on the specific needs of underrepresented populations can play a significant role in reducing maternal mortality rates. Tailoring interventions to meet individual community characteristics increases the likelihood of success in reaching vulnerable groups, ultimately improving maternal health outcomes nationwide.
Advocating for Maternal Health: Community Engagement and Support
Engaging communities in discussions about maternal health and advocating for policies that promote equitable healthcare access is crucial for addressing maternal mortality. Grassroots organizations and community leaders can work collaboratively to create awareness and provide resources that specifically cater to the needs of their constituencies. This localized approach often leads to more meaningful change as the advocacy reflects the unique challenges and necessities of each community.
Furthermore, fostering networks of support for new mothers can bolster mental health and overall well-being during the postpartum period. Completing the maternity journey involves engaging partners, family members, and healthcare providers to create strong support systems that prioritize maternal wellness. By focusing on community engagement and support, we can improve maternal health outcomes and effectively address preventable pregnancy-related deaths.
Frequently Asked Questions
What are the primary causes of maternal mortality in the U.S.?
Maternal mortality in the U.S. is predominantly caused by cardiovascular disease, which represents over 20% of pregnancy-related deaths. Other significant causes include complications related to pre-eclampsia, hemorrhage, and chronic health conditions exacerbated during pregnancy.
Why does the U.S. have such high maternal mortality rates compared to other high-income countries?
Maternal mortality rates in the U.S. are higher than in other high-income nations due to a combination of factors, such as a fragmented healthcare system, systemic inequities, and persistent racial and ethnic health disparities. Additionally, access to comprehensive prenatal and postpartum care varies significantly across states.
How do maternal health disparities affect pregnancy-related deaths in the U.S.?
Maternal health disparities significantly influence pregnancy-related deaths in the U.S., with racial and ethnic minority groups experiencing higher mortality rates. For example, American Indian and Alaska Native women face mortality rates nearly four times higher than white women, highlighting the urgent need for equitable healthcare policies.
What role does postpartum care play in reducing maternal mortality rates in the U.S.?
Postpartum care is crucial in reducing maternal mortality rates, as nearly one-third of pregnancy-related deaths occur after the initial postpartum period. Enhanced postpartum services can address potential complications that arise beyond the typical six-week recovery timeline, ensuring better long-term maternal health.
What are the statistics on U.S. pregnancy-related deaths, and how are they trending?
Recent U.S. pregnancy statistics show a troubling rise in maternal mortality rates, increasing from 25.3 deaths per 100,000 live births in 2018 to 32.6 in 2022. This trend indicates a need for immediate action to improve overall maternal health and address the factors contributing to rising death rates.
How does cardiovascular disease impact maternal health during pregnancy in the U.S.?
Cardiovascular disease, including hypertension and related conditions, has become a leading cause of maternal mortality in the U.S., affecting women at younger ages than previously seen. This shift underscores the importance of monitoring and managing chronic conditions throughout pregnancy.
What innovations are being proposed to improve outcomes related to maternal mortality in the U.S.?
To improve outcomes related to maternal mortality, experts suggest investing in public health infrastructure, enhancing prenatal and extended postpartum care, and addressing policy disparities between states. These innovations aim to ensure consistent and equitable healthcare access for all pregnant women.
Why is it important to consider late maternal deaths in discussions about maternal mortality in the U.S.?
Late maternal deaths, occurring between 42 days and 1 year postpartum, account for a significant portion of maternal mortality. Recognizing this time frame allows for a more comprehensive understanding of maternal health needs and the necessary healthcare services to support women during this crucial period.
What are the statistics reflecting racial disparities in maternal mortality in the U.S.?
Statistics reveal significant racial disparities in maternal mortality rates, with American Indian and Alaska Native women experiencing around 106.3 deaths per 100,000 live births, while white women face a rate of 27.6. These disparities illustrate the urgent need for targeted interventions and policies to ensure equitable care for all women.
How can better data tracking improve understanding of maternal mortality in the U.S.?
Improving data tracking of maternal deaths in the U.S. can enhance understanding and identification of trends related to maternal mortality. Since consistent tracking began in 2018, researchers have gained better insights into the causes and demographics of maternal deaths, allowing for targeted public health interventions.
| Key Point | Details |
|---|---|
| Rising Maternal Mortality Rates | The U.S. has the highest maternal mortality rate among high-income countries, with a notable increase from 2018 to 2022. |
| Disparities in Maternal Mortality | Significant disparities exist by state, race, and ethnicity; American Indian and Alaska Native women experience the highest rates. |
| Preventability of Deaths | Over 80% of pregnancy-related deaths are deemed preventable, highlighting the need for improved care. |
| Impact of COVID-19 | The highest increase in maternal mortality was observed in 2021, likely linked to the pandemic. |
| Leading Causes of Death | Cardiovascular disease is now the leading cause of pregnancy-related death, surpassing hemorrhage. |
| Importance of Postpartum Care | Late maternal deaths (42 days to 1 year postpartum) represent nearly a third of total mortality, emphasizing the need for extended care. |
| Need for Policy Reform | The study suggests a need for better healthcare policies and infrastructure at state levels to address disparities. |
Summary
Maternal mortality in the U.S. continues to be a pressing health issue, with alarming statistics indicating that many pregnancy-related deaths are preventable. As research shows an increase in these rates amid systemic inequality and healthcare disparities, comprehensive reforms are necessary to enhance both prenatal and postpartum care. Addressing the root causes of this trend is critical to ensuring the health and safety of mothers across the country.