Pediatric brain cancer prediction is revolutionizing the way we approach the diagnosis and management of childhood brain tumors. Recent advancements in artificial intelligence (AI) technology have shown promise in significantly enhancing the accuracy of predicting cancer recurrence, particularly in cases of pediatric gliomas. A groundbreaking study highlighted the efficacy of a novel AI tool, which leverages temporal learning to analyze multiple MRI scans over time, offering a more precise assessment of relapse risk than traditional methods. This innovative approach not only aids in earlier detection but also aims to reduce the psychological burden on young patients and their families. As researchers delve deeper into pediatric cancer research, the integration of AI in medicine emerges as a beacon of hope for improving outcomes in vulnerable populations.
The prediction of brain cancer in children, particularly regarding the likelihood of recurrence, has become a critical area of focus within the medical community. Utilizing cutting-edge technology and methodologies, experts are exploring the implications of artificial intelligence in analyzing longitudinal imaging data for pediatric tumors. By harnessing advanced algorithms to monitor changes in brain scans over time, researchers can develop more accurate forecasts for conditions like pediatric gliomas. This shift toward predictive analytics not only enhances patient care but also contributes significantly to the evolving landscape of pediatric cancer treatment strategies. As investigations continue, the promise of improved diagnostics and targeted interventions draws nearer, bolstering hope for affected families.
The Role of AI in Predicting Pediatric Brain Cancer Recurrence
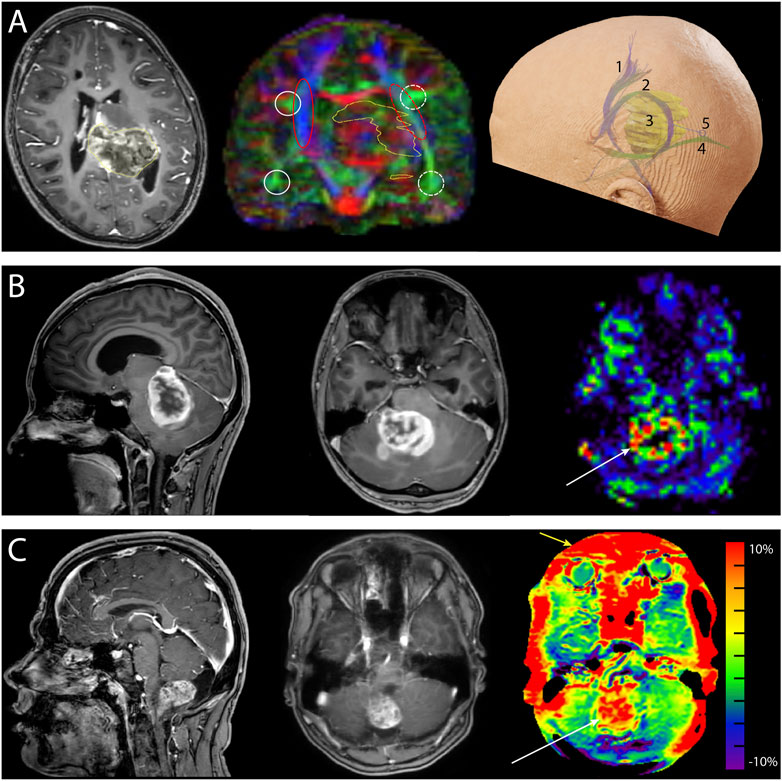
In recent years, AI technology has significantly transformed the landscape of medical diagnosis and treatment, particularly in pediatric oncology. The latest advances in AI algorithms have demonstrated a superior ability to predict relapse risk in pediatric brain cancer patients compared to traditional methods. Specifically, a study conducted by researchers at Mass General Brigham highlighted the effectiveness of a temporal learning AI tool that analyzed brain scans over time, providing a more nuanced understanding of pediatric gliomas. This innovative approach allows clinicians to identify patients who might be at greater risk for recurrence, thus tailoring follow-up care more effectively.
The AI model developed in the study utilizes a technique called temporal learning, which synthesizes data from various MR scans taken over a span of months after surgery. By looking at sequences of images rather than isolated scans, this model has achieved an impressive accuracy rate of 75-89% in predicting relapse risks for low or high-grade gliomas. This not only changes how pediatric brain cancer is monitored but also paves the way for potential breakthroughs in pediatric cancer research, enabling better-informed decision-making in clinical settings.
Improving Care for Pediatric Glioma Patients
The care management of pediatric glioma patients is undergoing a significant shift thanks to advancements in predictive analytics and AI technologies. Traditionally, children diagnosed with brain tumors have faced the anxiety of regular imaging follow-ups, a routine that can often be burdensome for both the children and their families. However, by adopting AI tools that predict the likelihood of cancer recurrence, healthcare providers may soon alleviate some of this stress. For instance, children determined to be at lower risk could potentially reduce the frequency of their imaging sessions, allowing them to focus more on recovery and less on medical appointments.
Moreover, the integration of AI in medicine highlights an essential shift toward personalized treatment strategies. With the ability to identify patients more likely to experience recurrence early, oncologists can initiate targeted adjuvant therapies proactively. This is especially crucial in the case of pediatric brain cancer, where timely intervention can make a significant difference in outcomes. As research continues to validate the efficacy of these AI models, the ultimate goal is to enhance the care continuum for young patients fighting pediatric cancer.
Furthermore, the cross-institutional collaboration exhibited in this study underscores the importance of joint efforts in the field of pediatric cancer research. By pooling resources and data, institutions like Boston Children’s Hospital and Dana-Farber are setting a precedent for how interdisciplinary partnerships can drive advancements in cancer care.
Temporal Learning AI: A Game Changer for Pediatric Oncology
Temporal learning AI represents a groundbreaking advancement in how brain imaging data is utilized in the field of pediatric oncology. Unlike conventional AI methods that rely on individual images to generate predictions, temporal learning provides a comprehensive analysis by interpreting sequences of scans over time. This innovative application is particularly pertinent in assessing pediatric gliomas, which typically require ongoing monitoring following treatment. The study underscored how this AI tool could effectively track subtle changes in patients’ conditions, greatly improving the accuracy of relapse predictions.
Researchers have noted that the integration of temporal learning into standard imaging protocols could lead to more precise evaluations of disease progression. By being able to analyze a series of scans, physicians can gain insight into the treatment efficacy and make informed decisions regarding treatment adjustments. This method not only enhances the reliability of predictions regarding recurrence but also signifies a move towards a more adaptive model of care that can respond dynamically to each patient’s journey.
The Future of AI in Pediatric Cancer Research
As the field of pediatric cancer research continues to evolve, the role of AI is becoming increasingly critical. The ability to harness vast amounts of imaging data and learn from it offers hospitals and research institutions the opportunity to dramatically change treatment protocols for young cancer patients. The insights gained from studies like the one at Mass General Brigham provide a foundation for future investigations into how AI can be used to predict outcomes in various types of pediatric malignancies, not just gliomas.
Furthermore, ongoing research in AI applications may uncover novel patterns in pediatric cancer recurrence, advancing our understanding of tumor biology. The potential for AI-driven tools to assist in early diagnosis, personalized medicine, and treatment effectiveness monitoring could revolutionize care in pediatric oncology, leading to improved outcomes for patients. This transition towards data-driven solutions represents a pivotal step that harnesses technology to better serve the needs of children battling cancer.
Challenges and Considerations in AI Implementation
While the potential benefits of AI in predicting pediatric brain cancer recurrence are significant, several challenges remain in the implementation of these tools in clinical settings. One of the primary concerns is ensuring the accuracy of AI predictions across diverse patient populations and varying healthcare infrastructures. As the initial studies have shown promising results, further validation across different clinical settings is essential for the wider adoption of AI technologies. This will involve addressing variability in scans, diverse healthcare access, and patient demographics.
Moreover, ethical considerations around privacy and data security must be prioritized. As AI systems require vast amounts of patient data for training, ensuring that this information is used responsibly and securely is paramount. Stakeholders in pediatric cancer research, including hospitals, regulatory agencies, and patient advocates, must collaborate to establish clear guidelines that prioritize patient safety while promoting technological advancement in treatment methodologies.
Pediatric Gliomas: Understanding Relapse Risks
Pediatric gliomas, while often treatable, pose a significant challenge due to the uncertain risk of recurrence. Understanding these risks is vital to providing effective treatment plans and managing patient care. Traditionally, the assessment of relapse risk has relied on a combination of histological analysis and imaging studies, but these methods have not always provided clear forecasts. The incorporation of AI predictive tools allows for a more nuanced evaluation of individual cases, potentially leading to improved risk stratification.
Researchers emphasize the need for ongoing studies to further explore the variances in glioma behavior among pediatric patients. Factors such as tumor location, genetic markers, and patient age can all influence the likelihood of recurrence. By integrating AI analysis into these investigations, the hope is to uncover deeper insights that could guide more personalized treatment strategies for young patients facing the challenges of brain cancer.
The Impact of AI on Patient Monitoring Practices
The advent of advanced AI tools in medical imaging is quantifiably reshaping the methodologies used in monitoring pediatric cancer patients post-treatment. With traditional imaging follow-up protocols often being resource-intensive and stressful for young patients, AI-enhanced monitoring represents a paradigm shift. By utilizing predictive analytics that assess multiple scans over time, clinicians can better gauge patient conditions without subjecting them to unnecessary anxiety.
This new approach not only has the potential to reduce the frequency of MRI scans for patients at lower risk of recurrence but could also streamline workflows in busy pediatric oncology departments. With quicker and more reliable analyses, healthcare teams can focus on providing care that is more responsive and tailored to each patient’s unique situation. The outcome of these innovations could herald a new era in pediatric cancer care, where patient experience and treatment efficacy are significantly enhanced.
Collaborative Efforts in Pediatric Cancer Research
The collaboration among various institutions, such as Mass General Brigham, Boston Children’s Hospital, and Dana-Farber, underscores the importance of collective efforts in advancing pediatric cancer research. These partnerships not only enable the pooling of resources but also facilitate the sharing of diverse expertise that can lead to innovative breakthroughs in understanding and treating pediatric gliomas. Such integrative research approaches are essential for tackling the complexities associated with pediatric malignancies.
Going forward, fostering inter-institutional collaborations will be crucial for accelerating research efforts aimed at understanding the prognosis of pediatric brain cancers. These alliances can yield larger datasets and enhanced study designs, which in turn can inform the development of AI tools tailored to identifying recurrence risks. Ultimately, these cooperative efforts may be instrumental in improving treatment outcomes and survival rates for affected children.
Future Directions and Innovations in Pediatric Oncology
Looking ahead, the integration of AI into pediatric oncology is poised to propel forward not only research but also clinical application. With emerging technologies continually reshaping diagnostic frameworks, there is a pressing need to adapt treatment protocols accordingly. The promise of AI-driven insights into pediatric brain cancer, particularly through refined understanding of gliomas, holds transformative potential for patient care.
Continued investment in research and development surrounding AI tools will be essential for harnessing their full capacity in predictive medicine. As studies validate the accuracy and effectiveness of these innovations, we can expect to see a ripple effect throughout pediatric cancer management practices, fostering a climate of hope and resilience for young patients and their families.
Frequently Asked Questions
How does pediatric brain cancer prediction using AI improve outcomes for glioma patients?
Pediatric brain cancer prediction utilizing AI enhances outcomes by accurately assessing the risk of recurrence in glioma patients. The AI tool analyzes multiple brain scans over time, employing a technique called temporal learning to identify subtle changes that indicate potential relapses, thus allowing for more proactive treatment approaches.
What advancements in pediatric cancer research have stemmed from AI in medicine regarding gliomas?
Advancements in pediatric cancer research, particularly in pediatric gliomas, have been significantly influenced by AI in medicine. This includes the development of robust predictive models that leverage temporal learning, enabling clinicians to forecast cancer recurrence with improved accuracy, ultimately informing treatment decisions and reducing unnecessary stress for families.
What is temporal learning AI and how does it apply to pediatric brain cancer prediction?
Temporal learning AI is a machine learning technique that sequentially analyzes multiple imaging data points over time. In pediatric brain cancer prediction, it allows the AI to recognize trends and changes across several MRI scans post-surgery, leading to a more dependable assessment of relapse risk in patients with brain tumors like gliomas.
What findings did the study on pediatric gliomas reveal about predicting brain cancer recurrence?
The study revealed that the AI model could predict brain cancer recurrence in pediatric gliomas with an accuracy of 75-89%, compared to 50% accuracy from traditional methods based on single images. This highlights the importance of using multiple scans to improve prediction reliability.
Why is predicting brain cancer recurrence important in pediatric patients?
Predicting brain cancer recurrence in pediatric patients is crucial because it enables timely intervention and personalized treatment strategies. By accurately forecasting who is at risk, healthcare providers can tailor follow-up care, minimize unnecessary stress on patients and families, and optimize outcomes for children battling pediatric gliomas.
How can AI tools change the landscape of follow-up care in pediatric brain cancer treatment?
AI tools can revolutionize follow-up care by reducing the frequency of imaging for low-risk pediatric brain cancer patients while ensuring that high-risk patients receive timely and targeted therapies. This shifts the emphasis from routine scans to risk-based personalized care, improving both the experience and outcomes for pediatric patients.
What role does artificial intelligence play in enhancing accuracy for pediatric brain cancer prediction?
Artificial intelligence enhances accuracy in pediatric brain cancer prediction through advanced analytical capabilities, such as identifying patterns in longitudinal imaging data. This results in better identification of at-risk patients and allows for more effective, individualized treatment planning.
| Key Points |
|---|
| An AI tool developed to predict relapse risk in pediatric patients with brain cancer has shown improved accuracy compared to traditional methods. |
| The study emphasizes the importance of early identification of relapse risk in children with gliomas to enhance patient care. |
| Temporal learning technique was used in AI to analyze multiple MRI scans over time, significantly improving predictive capabilities. |
| Results indicate a prediction accuracy of 75-89% for glioma recurrence within one year post-treatment. |
| Further validation and clinical trials are necessary to implement AI predictions in routine care. |
Summary
Pediatric brain cancer prediction is significantly enhanced through the use of AI technology, as shown in a recent study by researchers at Mass General Brigham. The study highlighted that an AI model utilizing temporal learning achieved a remarkable accuracy rate of 75-89% in predicting the risk of relapse in children with gliomas, surpassing traditional single-scan methods. This advancement indicates the potential for better monitoring and early intervention in pediatric patients, ultimately aiming to improve their long-term health outcomes.