
Bile Imbalance and Liver Cancer: Key Findings Revealed
Bile imbalance, a significant factor in liver cancer, has emerged as a critical area of research in understanding hepatocellular carcinoma (HCC), the most prevalent form of this disease. Recent studies indicate that disturbances in bile acid metabolism can set off a cascade of liver injuries, ultimately leading to cancerous growths. The intricate relationship between bile acids and cancer highlights the importance of examining molecular mechanisms, such as the YAP-FXR interaction, that contribute to liver pathology. Researchers are now exploring innovative liver cancer treatment options that target these metabolic pathways, potentially offering new hope for patients. As our understanding deepens, the link between bile acids and cancer not only frames new investigative avenues but also emphasizes the urgency of addressing bile imbalance in preventive strategies.
The issue of bile imbalance, related to liver malignancies, is gaining traction in medical research. Disruptions in bile production and regulation have been implicated in various liver diseases, including hepatocellular carcinoma (HCC). Understanding how these bile acids function and interact within the body’s systems is essential for developing effective liver cancer therapies. Moreover, the exploration of bile acid dynamics, along with its metabolic effects, is vital for future clinical interventions geared at reducing cancer risks. By investigating the roles of key regulators such as YAP and FXR, we can uncover new therapeutic possibilities that target bile metabolism and its influence on liver health.
Understanding Bile Imbalance and Its Impact on Liver Health
Bile health plays a pivotal role in the overall functioning of the liver, where bile acids not only aid in fat digestion but also regulate various metabolic processes. An imbalance in bile can lead to serious liver issues, including hepatocellular carcinoma (HCC), the most prevalent form of liver cancer. Research indicates that dysregulation of bile acid production harms liver tissues, leading to inflammation and potentially cancerous growth. Hence, monitoring bile acid levels is critical for early detection and prevention of liver diseases.
Recent findings have linked bile acid metabolism to important regulatory pathways such as the Hippo/YAP pathway. When bile acids are produced in excess, as seen in cases of bile imbalance, they can disrupt essential liver functions, prompting further investigation into interventions that may normalize these levels. Understanding the connection between bile acid levels and liver cancer opens new avenues for liver cancer treatment, especially through targeted therapies that aim to restore metabolic balance.
Frequently Asked Questions
How is bile imbalance related to liver cancer treatment?
Bile imbalance has been shown to play a significant role in liver cancer treatment by influencing tumor promotion through pathways like the Hippo/YAP interaction. By targeting bile acid metabolism and enhancing fxr function, new therapies may emerge to manage hepatocellular carcinoma (HCC) more effectively.
What role do bile acids play in cancer progression, particularly in liver cancer?
Bile acids serve not only as digestive agents but also regulate metabolic processes. Imbalances in bile acids can lead to liver injury and inflammation, which are key precursors to hepatocellular carcinoma (HCC), linking bile acid metabolism directly to cancer progression.
What is the significance of the Hippo/YAP pathway in bile acid metabolism and liver cancer?
The Hippo/YAP pathway is crucial for cell growth regulation and has been found to repress FXR, a bile acid sensor. This disruption leads to overproduction of bile acids, which is linked to liver fibrosis and hepatocellular carcinoma (HCC).
How does the YAP-FXR interaction affect bile acid levels in liver cancer patients?
In liver cancer patients, YAP activation can impair FXR function, leading to excessive bile acid build-up in the liver. This imbalance contributes to liver damage and the progression to hepatocellular carcinoma (HCC).
What research is being done on bile acids and cancer?
Current HCC research focuses on the role of bile acids in liver cancer development, particularly how their imbalance impacts liver metabolism and how targeting the FXR might provide new treatment avenues for hepatocellular carcinoma.
Can targeting bile acid metabolism lead to new therapies for liver cancer?
Yes, targeting bile acid metabolism, especially through enhancing FXR function or promoting bile acid excretion, could lead to innovative therapies for liver cancer treatment by alleviating the damaging effects of bile imbalance.
What findings were published in relation to bile imbalance and liver cancer in Nature Communications?
Recent findings indicate that an imbalance in bile acids can trigger liver diseases, including hepatocellular carcinoma (HCC), by disrupting bile acid metabolism through the YAP-FXR interaction, highlighting potential intervention points for liver cancer treatment.
How does bile acid homeostasis influence the development of hepatocellular carcinoma?
Bile acid homeostasis is critical; when disrupted, it leads to overproduction of bile acids that contributes to inflammation and fibrosis, setting the stage for the development of hepatocellular carcinoma (HCC).
| Key Point | Details |
|---|---|
| Bile Acid Imbalance | An imbalance in bile acids can lead to liver diseases, particularly hepatocellular carcinoma (HCC), the most common type of liver cancer. |
| Molecular Switch Identified | A key molecular switch, the YAP protein, has been identified that regulates bile acid metabolism. |
| Role of YAP | Surprisingly, YAP promotes tumor formation by inhibiting FXR (Farnesoid X receptor) essential for bile acid homeostasis. |
| Therapeutic Implications | Blocking YAP’s repressive effects or stimulating FXR could lead to new liver cancer treatments. |
| Research Support | The study was supported by the National Institutes of Health and the National Cancer Institute. |
Summary
Bile imbalance and liver cancer are intricately linked, as evidenced by recent research revealing how disrupted bile acid metabolism can trigger severe liver diseases, including hepatocellular carcinoma (HCC). The identification of the YAP protein as a molecular switch highlights the potential for new therapeutic strategies that target bile acid regulation, offering hope for more effective treatments against liver cancer.

Gene Editing Advancements: A Breakthrough in Medicine
Gene editing advancements are at the forefront of revolutionary changes in medicine, offering unprecedented opportunities to treat and potentially cure genetic diseases. Recent developments in CRISPR technology, along with innovations such as base editing and prime editing, have significantly enhanced our ability to alter genetic material with precision. Pioneered by experts like David Liu, these techniques allow scientists to directly address the mutations responsible for various ailments, marking a new era in therapeutic interventions. As clinical trials continue to demonstrate remarkable outcomes, it is clear that these advancements are transforming how we understand and treat hereditary conditions. The journey of gene editing is not just a scientific endeavor; it embodies hope for millions affected by genetic disorders worldwide.
The field of genetic modification has witnessed groundbreaking progress that is reshaping the landscape of healthcare. Alternative methods, including genetic engineering and molecular editing technologies, are being developed to tackle the complexities of genetic disorders. Innovators in the scientific community, like those working with CRISPR-based systems, are leveraging their findings to create robust solutions tailored to individual genetic profiles. This shift towards precise genetic alterations signifies a major step in modern medicine, enhancing our ability to manage and potentially reverse the impact of genetic anomalies. As researchers unveil new possibilities, the implications for disease management and health outcomes are becoming increasingly promising.
The Rise of Gene Editing Advancements
In recent years, gene editing advancements have made remarkable strides, particularly with the introduction of base editing and prime editing technologies. These innovations have transformed how scientists approach genetic diseases that were once deemed untreatable. Base editing, which enables precise modifications at specific spots in DNA, allows for an unprecedented level of control over genetic alterations. This approach, developed by David Liu and his team, is demonstrating the capacity to correct mutations without the risks associated with traditional gene-editing methods, such as the CRISPR-Cas9 technique that cuts DNA strands.
Prime editing represents another significant leap in the field, functioning more like a word processor for DNA. It allows researchers to replace faulty DNA sequences with correct ones without causing double-strand breaks, which often lead to unintended consequences. This groundbreaking technology has opened new avenues for the treatment of a diverse range of genetic disorders. With ongoing clinical trials, we are witnessing the tangible impact of these gene editing advancements in therapeutic settings. Liu’s innovative work signifies not just a technological triumph but a beacon of hope for millions affected by genetic diseases.
The Impact of CRISPR Technology
CRISPR technology revolutionized genetic research when it was discovered that bacteria use it as a defense mechanism against viruses. This system provides a way to edit genes with incredible precision, and it sparked a wave of enthusiasm and exploration in the scientific community. David Liu’s contributions have expanded this foundation, moving beyond CRISPR’s original applications to refine methods of gene correction. The development of base editing and prime editing can be traced back to the insights gained from studying CRISPR, showcasing how basic scientific research can lead to groundbreaking technological advancements.
The implications of CRISPR are vast, impacting not only medicine but agricultural practices and biodiversity conservation as well. In the realm of genetic diseases, CRISPR-based technologies have the potential to address some of the most persistent issues in healthcare. Liu emphasizes that it’s vital for researchers to ensure the safety of these tools in clinical applications, as society grapples with ethical considerations and the potential for misuse. By navigating these challenges, the scientific community can harness the powers of CRISPR technology responsibly, leading to a healthier future for all.
Exploring Base Editing Techniques
Base editing is a transformative gene-editing technique that allows for targeted alteration of DNA bases without cutting the DNA strands. This approach enables scientists to rectify point mutations—variations in a single DNA base pair—that are responsible for many genetic diseases. By offering a more refined method of gene modulation, base editing minimizes errors and unintended consequences, thereby enhancing the safety of therapeutic interventions. As highlighted by David Liu’s work, transforming our understanding of how to manipulate DNA brings new hope to patients suffering from conditions like sickle cell disease and beta-thalassemia.
The precision of base editing makes it a compelling tool in the fight against genetic disorders. For example, recent clinical trials have demonstrated the effectiveness of this technique in ensuring long-term remission in patients previously reliant on medication. By correcting the root cause of these diseases at their genetic source, base editing holds the promise of transitioning from symptom management to disease resolution. As ongoing research continues to push the boundaries of what is possible, the future of base editing shines brightly in the landscape of genetic medicine.
Prime Editing: The Future of Genetic Correction
Prime editing is often touted as the next frontier in gene editing, thanks to its remarkable ability to introduce precise changes to DNA sequences. Liu’s pioneering work resulted in a technology that not only edits genes but also does so with unparalleled finesse. Unlike CRISPR and traditional gene-editing methods, prime editing acts like a word processor, allowing scientists to search for specific sequences of DNA and replace them accurately, addressing issues like extra or missing letters in the genetic code. This next-generation tool heralds a new era of possibilities for correcting inherited genetic disorders.
The implications of prime editing extend far beyond its technical capabilities. With ongoing research and clinical trials confirming its efficacy, prime editing is positioning itself as a cornerstone of future therapeutics. Patients with various genetic diseases may soon experience the benefits of these innovations, potentially leading to results that could redefine long-term outcomes. By marrying scientific rigor with technological advancement, prime editing is set to make substantial contributions to the field of genetic medicine, carrying the promise of transformative treatments to those in need.
Advances in Therapeutic Applications
The advances in gene editing techniques like base editing and prime editing are opening new doors for therapeutic applications. For instance, in clinical trials that utilize these technologies, patients are being treated for diseases previously deemed unmanageable. Notably, the case of Alyssa Tapley showcases how these innovations have resulted in successful remission of T-cell leukemia, providing a lifeline to many who suffer from genetic afflictions. By demonstrating tangible results, these therapeutic applications not only inspire confidence but also emphasize the importance of advancing gene editing methodologies.
There are at least 18 clinical trials currently underway that employ base editing or prime editing to treat various diseases. These trials are critical as they bridge the gap between laboratory research and real-world medical applications. Moving forward, the data gleaned from these studies will be essential in understanding the long-term impacts of gene editing on health outcomes. The advances made today are shaping the future of medicine, and the hope is to create treatments that not only improve quality of life but potentially cure genetic diseases.
Overcoming Challenges in Gene Editing
Despite the tremendous promise of gene editing technologies, several challenges remain. One of the primary hurdles is ensuring the safety and efficacy of these treatments before they can be widely adopted. As David Liu mentions, it is crucial for researchers to conduct thorough testing to minimize the risks associated with these novel therapies. Regulatory considerations are also paramount, as successful application in clinical settings requires rigorous oversight to protect patients and uphold ethical standards.
Moreover, there are inherent societal challenges regarding the perception and acceptance of gene editing. Misunderstandings and ethical dilemmas surrounding genetic manipulation could hinder progress in research and implementation. Engaging with communities and providing clear communication about the benefits and risks involved in gene editing is essential for fostering public trust. As scientists, educators, and policymakers work together to navigate these challenges, the future of gene editing can become a collaborative effort grounded in progress and responsibility.
The Role of Basic Science in Gene Editing
The foundation of gene editing advancements lies in the realm of basic scientific research. David Liu emphasizes that discoveries in basic science often reveal fundamental truths about genetic mechanisms, paving the way for technological innovations. It was thorough investigation into DNA structure and function over decades that led to the momentous discovery of CRISPR technology, demonstrating how curiosity-driven science can yield transformative applications. Without this foundational work, breakthroughs like base and prime editing may not have materialized.
Basic science is vital because it seeks to understand the unknown and pushes the boundaries of knowledge without the immediate pressure of application. This foundational understanding of genetic systems has led to the development of tools that can accurately manipulate the genetic code. Liu’s advocacy for basic research stresses that the pursuit of knowledge for its own sake can lead to the remarkable advances we are seeing in gene editing and its applications in fields ranging from healthcare to biotechnology.
Future Considerations in Genetic Research
As gene editing continues to evolve, future considerations must address both the scientific and ethical dimensions of this powerful technology. Researchers like Liu express concern about maintaining a robust partnership between academia and governmental agencies to nurture the next generation of scientists. The current landscape poses numerous challenges that threaten to stifle innovation and collaboration—dynamics that are essential for breakthroughs in understanding and medical applications of genetic technologies.
The future of genetic research must also engage public dialogue about the implications of gene editing advancements. By fostering open conversations about the benefits and potential risks, scientists can better prepare society for the changes that these technologies will bring. Addressing ethical concerns and ensuring equitable access to gene therapies will be critical as these innovations become more integrated into our healthcare systems. In striving for a responsible and inclusive approach, the benefits of gene editing can extend to all, ultimately shaping a more equitable future.
Frequently Asked Questions
What are the latest advancements in gene editing technologies like CRISPR and base editing?
Recent advancements in gene editing technologies, particularly CRISPR, base editing, and prime editing, have transformed the field of genetics. CRISPR technology continues to be a cornerstone, providing precise cuts in DNA for gene disruption. Base editing, developed by scientists like David Liu, allows for direct single base changes without needing to cut the double helix, making it ideal for correcting mutations that cause genetic diseases. Prime editing takes this further by enabling more complex edits, such as adding, deleting, or replacing DNA sequences, effectively functioning like a word processor for genomic sequences.
How is David Liu’s work with base editing impacting the treatment of genetic diseases?
David Liu’s work on base editing has significant implications for the treatment of genetic diseases. His approach allows for precise corrections of common mutations associated with various conditions by directly altering the DNA bases. This groundbreaking technology has already led to clinical trials where patients with genetic disorders, such as T-cell leukemia, have shown remarkable recovery outcomes after treatment with base editing, showcasing its potential as a powerful tool in modern medicine.
What are the differences between CRISPR, base editing, and prime editing in gene editing?
CRISPR, base editing, and prime editing serve different roles in gene editing. CRISPR technology involves cutting DNA strands to disrupt genes, which can sometimes lead to unintended consequences. Base editing, pioneered by David Liu, modifies DNA bases directly without cutting the DNA, thus minimizing potential off-target effects and allowing for precise corrections of genetic mutations. Prime editing is an even more advanced technique that enables users to search and replace DNA sequences accurately, akin to using a text editor, making it possible to address a broader array of genetic mutations.
What role does base editing play in clinical trials for genetic disease treatment?
Base editing plays a crucial role in clinical trials aiming to treat genetic diseases. As of now, numerous clinical trials are utilizing base editing to address various conditions. Notably, some patients treated with base editing technologies have reported significant improvements in their health, leading to a reduction in symptoms and the need for medications. This innovative approach is reshaping our understanding of potential therapies for previously untreatable genetic conditions.
How has CRISPR technology paved the way for advancements in genetic disease treatment?
CRISPR technology has been foundational in advancing the treatment of genetic diseases. Its discovery ignited research into gene editing, leading to the development of more refined techniques like base editing and prime editing. By enabling targeted genetic modifications, CRISPR has empowered scientists to explore therapeutic interventions for a wide array of genetic disorders, establishing a platform from which novel treatments are continually emerging.
What are the future prospects of gene editing advancements in healthcare?
The future prospects of gene editing advancements in healthcare are incredibly promising. With ongoing research and breakthroughs in technologies like CRISPR, base editing, and prime editing, the potential to effectively treat and even cure genetic diseases is growing. As these techniques advance, we can expect more clinical applications in personalized medicine, providing tailored treatments that address the genetic underpinnings of various ailments, thus revolutionizing healthcare delivery.
| Key Points | Details |
|---|---|
| Novel Gene Editing Technologies | Base editing and prime editing are innovative methods developed to correct genetic diseases by targeting single nucleotide changes. |
| Success Story: Alyssa Tapley | At age 13, Tapley’s T-cell leukemia was treated successfully with base editing technology in a clinical trial, marking a significant scientific breakthrough. |
| The Role of David Liu | David Liu, a leading scientist, emphasizes the ethical responsibility in ensuring the safety and efficacy of gene-editing techniques. |
| Historical Significance of CRISPR | The journey of CRISPR’s discovery from basic science in E. coli to its application in gene editing illustrates the importance of fundamental research. |
| Clinical Trials | As of 2025, there are at least 18 clinical trials exploring base and prime editing for genetic diseases, demonstrating real-world applications. |
Summary
Gene editing advancements have significantly changed the landscape of medical treatment, particularly for genetic diseases. The development of base editing and prime editing technologies provides a new pathway to correct genetic mutations at a molecular level. With successful cases like Alyssa Tapley’s, these innovations demonstrate the potential to transform patient outcomes and offer hope to millions suffering from genetic disorders.
Maternal Mortality in the U.S.: A Rising Concern
Maternal mortality in the U.S. remains a critical public health concern, as recent data highlights the alarming rise in pregnancy-related deaths. Despite being a high-income nation, the U.S. leads its peers with a maternal mortality rate that has not only persisted but escalated in recent years. A staggering 80% of these deaths are deemed preventable, spotlighting significant maternal health disparities across different states and demographics. The rise in cardiovascular disease as a leading concern during pregnancy further exacerbates these statistics, emphasizing the need for comprehensive prenatal and postpartum care. Addressing these issues is paramount to ensuring healthier outcomes for mothers and their newborns in an era marked by rising U.S. pregnancy statistics.
In recent years, the issue of maternal mortality in America’s healthcare landscape has gained urgent attention, with increasing instances of pregnancy-related fatalities. Terms like maternal death rates and health inequities are prevalent as researchers dissect the complex factors contributing to this troubling trend. Several recent studies indicate a correlation between cardiovascular conditions and pregnancy, leading to greater fatalities among expectant mothers. Furthermore, disparities in access to quality maternal health care reveal alarming patterns, particularly among marginalized communities. Thus, the emphasis on effective postpartum care becomes crucial in addressing the multifaceted challenges surrounding maternal health and reducing preventable fatalities.
The Alarming Increase in Maternal Mortality in the U.S.
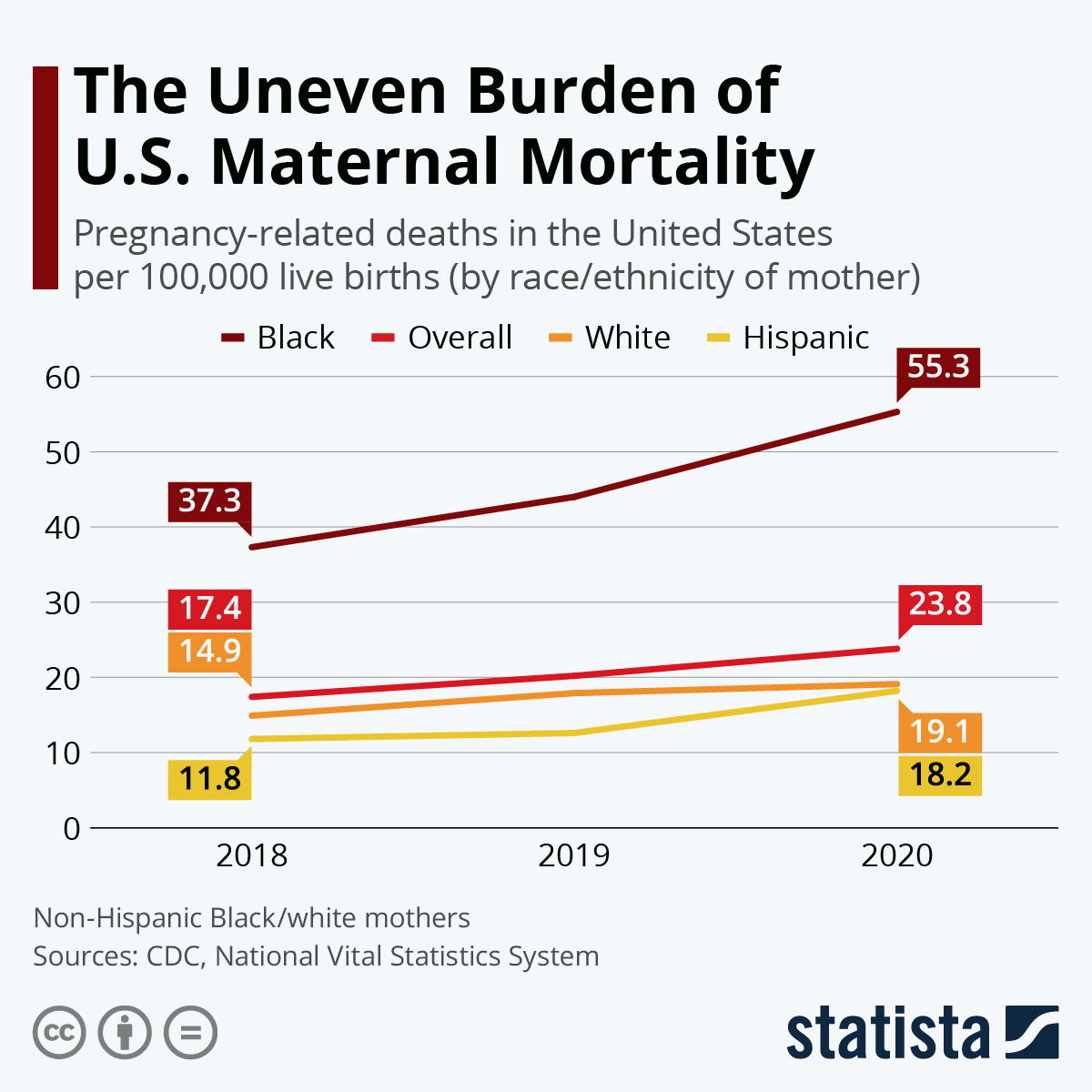
The United States boasts the highest maternal mortality rate among high-income nations, and recent studies reveal that the situation is worsening. From 2018 to 2022, the maternal mortality rate saw a significant increase, with particularly sharp spikes noted during the COVID-19 pandemic. This alarming trend illustrates the urgent need for effective interventions to address preventable pregnancy-related deaths, as over 80% of these deaths are deemed preventable. The call for improved prenatal care and comprehensive postpartum support has never been more critical, as we strive to reduce this troubling statistic.
Disparities in maternal health further exacerbate the issue, with racial and ethnic minorities facing disproportionate challenges. For instance, American Indian and Alaska Native women experience mortality rates nearly four times higher than their white counterparts. These stark differences highlight the systemic flaws in the healthcare system that contribute to maternal mortality in the U.S. It is imperative that we work to rectify these disparities through targeted policies and initiatives that ensure equitable access to quality maternal healthcare.
Understanding Pregnancy-Related Deaths: Causes and Disparities
Pregnancy-related deaths can arise from various causes, with cardiovascular disease emerging as one of the leading threats to maternal health. This shift from historical causes, such as hemorrhage, to chronic conditions like hypertension and heart disease indicates a concerning trend of deteriorating maternal health among diverse demographics. Researchers have found that younger populations are now expressing these chronic conditions at alarming rates, posing significant risks during pregnancy.
Maternity care deserts and inequitable healthcare access further exacerbate the already significant maternal health disparities. Many individuals, especially from marginalized communities, find it challenging to access necessary prenatal care and postpartum resources. This leads to insufficient monitoring, delayed treatments, and ultimately higher mortality rates. Addressing these disparities is essential for fostering a maternal health environment where all women receive the care they deserve throughout the entire pregnancy continuum.
Postpartum Care Importance: A Continuous Journey
Postpartum care should be recognized as a critical phase for maternal health, extending beyond the conventional six-week checkup. Recent studies indicate that nearly a third of maternal deaths occur after the initial postpartum period, particularly emphasizing the need for ongoing healthcare after childbirth. By expanding the timeframe in which postpartum health is monitored, healthcare providers can intervene more effectively and prevent potential complications.
Investing in comprehensive postpartum care not only allows for better management of physical health but also addresses mental health challenges that many new mothers face. Improved support systems during this vulnerable time can significantly enhance long-term maternal and infant health outcomes. As more attention is given to the postpartum experience, the emphasis on creating a continuum of care for mothers becomes increasingly clear—setting a foundation for healthier families.
The Role of Cardiovascular Disease in Maternal Health
Cardiovascular disease is now recognized as a leading cause of pregnancy-related death in the United States, accounting for over 20% of fatalities. The increase in rates among younger women, particularly those in the 25 to 39 age range, underscores the necessity for proactive monitoring and management of chronic health issues before and during pregnancy. As chronic conditions like hypertension become prevalent in younger populations, it’s essential for healthcare providers to assess these risks early on.
Furthermore, the impact of cardiovascular health on pregnancy outcomes cannot be overstated. The transition to a more cardiovascular-focused approach in maternal health care is vital in reducing pregnancy-related mortality rates. By prioritizing education about heart health and creating targeted interventions for at-risk populations, healthcare systems can make considerable progress in safeguarding mothers’ lives.
Preventing Maternal Mortality: Policy Changes Needed
Amid rising maternal mortality rates, there is a pressing need for comprehensive policy changes to address the underlying issues affecting maternal health. The disparities highlighted in recent studies reveal that some states perform significantly better than others, indicating that state-level policies and healthcare practices play a pivotal role. Implementing effective interventions tailored to each state’s unique challenges can drastically alter the maternal health landscape in the U.S.
Beyond addressing state disparities, investing in public health infrastructure is crucial for tracking and improving maternal health outcomes. Without adequate data collection and analysis, as seen in the recent increase in maternal mortality rates, informed policy-making becomes virtually impossible. Advocacy for enhanced research funding and a focus on maternal health will ensure we take meaningful steps towards improving care for all birthing individuals.
The Impact of Racial Disparities in Maternal Health
Racial disparities in maternal mortality rates are profound, with marginalized communities facing far greater risks than their white counterparts. Studies show that American Indian and Alaska Native women experience mortality rates nearly four times higher than white women. These alarming statistics highlight the critical role systemic bias and healthcare inequities play in exacerbating the crisis in maternal health.
Addressing these disparities necessitates a multifaceted approach, including policy reform and enhanced training for healthcare professionals on implicit biases. By prioritizing culturally competent care and ensuring equitable access to resources, we can work towards a healthcare landscape that provides fair and just maternal health outcomes for all women, regardless of their racial or ethnic background.
The Importance of Comprehensive Maternal Health Research
A critical aspect of improving maternal health outcomes lies in ongoing research and data collection. Until recently, the United States lacked a reliable national system for tracking pregnancy-related deaths, making it difficult to identify patterns and develop effective interventions. With the establishment of a standardized pregnancy checkbox on death certificates, future research looks promising, yet continued investment and commitment are required to ensure quality data is collected and analyzed.
Moreover, research not only informs policy but also drives innovation in maternal healthcare practices. By understanding the complexities of maternal health challenges, including those rooted in socioeconomic factors or chronic conditions, researchers can develop targeted solutions that address unique populations’ needs. This commitment to understanding and managing maternal mortality through rigorous research is essential to achieving sustainable improvements.
Innovative Solutions to Combat Maternal Mortality
Innovative solutions must be employed to address the increasing rates of maternal mortality in the U.S. From improving access to telehealth services for prenatal and postpartum care to ensuring quality education for healthcare providers, creative strategies can significantly influence maternal health outcomes. By leveraging technology, far-reaching benefits can be realized in terms of accessibility, effectiveness of care, and patient engagement.
Additionally, community-based programs that focus on the specific needs of underrepresented populations can play a significant role in reducing maternal mortality rates. Tailoring interventions to meet individual community characteristics increases the likelihood of success in reaching vulnerable groups, ultimately improving maternal health outcomes nationwide.
Advocating for Maternal Health: Community Engagement and Support
Engaging communities in discussions about maternal health and advocating for policies that promote equitable healthcare access is crucial for addressing maternal mortality. Grassroots organizations and community leaders can work collaboratively to create awareness and provide resources that specifically cater to the needs of their constituencies. This localized approach often leads to more meaningful change as the advocacy reflects the unique challenges and necessities of each community.
Furthermore, fostering networks of support for new mothers can bolster mental health and overall well-being during the postpartum period. Completing the maternity journey involves engaging partners, family members, and healthcare providers to create strong support systems that prioritize maternal wellness. By focusing on community engagement and support, we can improve maternal health outcomes and effectively address preventable pregnancy-related deaths.
Frequently Asked Questions
What are the primary causes of maternal mortality in the U.S.?
Maternal mortality in the U.S. is predominantly caused by cardiovascular disease, which represents over 20% of pregnancy-related deaths. Other significant causes include complications related to pre-eclampsia, hemorrhage, and chronic health conditions exacerbated during pregnancy.
Why does the U.S. have such high maternal mortality rates compared to other high-income countries?
Maternal mortality rates in the U.S. are higher than in other high-income nations due to a combination of factors, such as a fragmented healthcare system, systemic inequities, and persistent racial and ethnic health disparities. Additionally, access to comprehensive prenatal and postpartum care varies significantly across states.
How do maternal health disparities affect pregnancy-related deaths in the U.S.?
Maternal health disparities significantly influence pregnancy-related deaths in the U.S., with racial and ethnic minority groups experiencing higher mortality rates. For example, American Indian and Alaska Native women face mortality rates nearly four times higher than white women, highlighting the urgent need for equitable healthcare policies.
What role does postpartum care play in reducing maternal mortality rates in the U.S.?
Postpartum care is crucial in reducing maternal mortality rates, as nearly one-third of pregnancy-related deaths occur after the initial postpartum period. Enhanced postpartum services can address potential complications that arise beyond the typical six-week recovery timeline, ensuring better long-term maternal health.
What are the statistics on U.S. pregnancy-related deaths, and how are they trending?
Recent U.S. pregnancy statistics show a troubling rise in maternal mortality rates, increasing from 25.3 deaths per 100,000 live births in 2018 to 32.6 in 2022. This trend indicates a need for immediate action to improve overall maternal health and address the factors contributing to rising death rates.
How does cardiovascular disease impact maternal health during pregnancy in the U.S.?
Cardiovascular disease, including hypertension and related conditions, has become a leading cause of maternal mortality in the U.S., affecting women at younger ages than previously seen. This shift underscores the importance of monitoring and managing chronic conditions throughout pregnancy.
What innovations are being proposed to improve outcomes related to maternal mortality in the U.S.?
To improve outcomes related to maternal mortality, experts suggest investing in public health infrastructure, enhancing prenatal and extended postpartum care, and addressing policy disparities between states. These innovations aim to ensure consistent and equitable healthcare access for all pregnant women.
Why is it important to consider late maternal deaths in discussions about maternal mortality in the U.S.?
Late maternal deaths, occurring between 42 days and 1 year postpartum, account for a significant portion of maternal mortality. Recognizing this time frame allows for a more comprehensive understanding of maternal health needs and the necessary healthcare services to support women during this crucial period.
What are the statistics reflecting racial disparities in maternal mortality in the U.S.?
Statistics reveal significant racial disparities in maternal mortality rates, with American Indian and Alaska Native women experiencing around 106.3 deaths per 100,000 live births, while white women face a rate of 27.6. These disparities illustrate the urgent need for targeted interventions and policies to ensure equitable care for all women.
How can better data tracking improve understanding of maternal mortality in the U.S.?
Improving data tracking of maternal deaths in the U.S. can enhance understanding and identification of trends related to maternal mortality. Since consistent tracking began in 2018, researchers have gained better insights into the causes and demographics of maternal deaths, allowing for targeted public health interventions.
| Key Point | Details |
|---|---|
| Rising Maternal Mortality Rates | The U.S. has the highest maternal mortality rate among high-income countries, with a notable increase from 2018 to 2022. |
| Disparities in Maternal Mortality | Significant disparities exist by state, race, and ethnicity; American Indian and Alaska Native women experience the highest rates. |
| Preventability of Deaths | Over 80% of pregnancy-related deaths are deemed preventable, highlighting the need for improved care. |
| Impact of COVID-19 | The highest increase in maternal mortality was observed in 2021, likely linked to the pandemic. |
| Leading Causes of Death | Cardiovascular disease is now the leading cause of pregnancy-related death, surpassing hemorrhage. |
| Importance of Postpartum Care | Late maternal deaths (42 days to 1 year postpartum) represent nearly a third of total mortality, emphasizing the need for extended care. |
| Need for Policy Reform | The study suggests a need for better healthcare policies and infrastructure at state levels to address disparities. |
Summary
Maternal mortality in the U.S. continues to be a pressing health issue, with alarming statistics indicating that many pregnancy-related deaths are preventable. As research shows an increase in these rates amid systemic inequality and healthcare disparities, comprehensive reforms are necessary to enhance both prenatal and postpartum care. Addressing the root causes of this trend is critical to ensuring the health and safety of mothers across the country.

Boston Marathon Mental Health: Exploring Runners’ Journeys
The Boston Marathon has become more than just a race; it stands as a testament to the powerful connection between physical endurance and mental health. Mental health support during events like the Boston Marathon is crucial, as the triumphs and struggles of marathon finishers highlight the profound psychological benefits of running. With the rigorous training required to complete 26.2 miles, runners often discover invaluable insights into their own resilience and self-worth. The Boston Marathon not only fosters community spirit but also serves as a motivational platform for those seeking marathon training motivation amidst their personal challenges. Understanding the role of running psychology can enhance the overall experience, turning the marathon into a journey of healing and self-discovery.
When we discuss the psychological aspects of long-distance running, particularly in events like the Boston Marathon, we delve into a realm where mental fortitude meets physical challenge. This iconic race offers participants not only a chance to achieve a personal goal but also an opportunity to engage in meaningful self-reflection and emotional growth. For many, the act of preparing for such a demanding event serves as a motivational beacon, placing their mental health at the forefront of their training routine. From instances of camaraderie among runners to individual stories of perseverance, the significance of mental well-being cannot be overstated, as it often shapes the experiences of those crossing the finish line. Recognizing how marathon participation impacts mental health forms a crucial part of our understanding of this venerable event.
The Importance of Mental Health Support in Marathon Training
Mental health support plays an essential role in marathon training, especially for participants in high-stakes events like the Boston Marathon. The rigorous demands of preparing for a race can take a toll on an individual’s mental health, often leading to anxiety or feelings of inadequacy. Having access to mental health professionals during training helps runners navigate these psychological challenges, allowing them to cope better with the pressures they face. With the right support, runners can find motivation and strategies to maintain a positive mindset, which is crucial for their overall performance.
The Boston Marathon, in particular, highlights the significance of mental health support for its participants. As runners prepare for the race, they often battle self-doubt and other emotional hurdles that can affect not only their training but also how they approach the race itself. By integrating mental health resources into their preparation, participants can enhance their psychological resilience, leading to improved race-day performance. These mental health strategies not only bolster their capabilities as athletes but also contribute to their overall well-being.
Psychological Benefits of Running: More than Just Physical Gains
Engaging in running has numerous psychological benefits that extend beyond physical fitness. Runners often report feeling a significant reduction in stress and anxiety levels after a good workout. The Boston Marathon, for instance, serves as a case study for the psychological uplift that running can provide. Participants find joy and fulfillment in pushing their boundaries while simultaneously fostering a community spirit. As they train together, they forge connections with others who share similar goals, ultimately enhancing their mental health.
Furthermore, running instills a sense of accomplishment, especially when cross the Boston Marathon finish line. Completing a marathon signifies not just physical endurance but also mental grit. The euphoria that follows is often a powerful motivator for runners, leaving them feeling invincible. This positive reinforcement encourages individuals to pursue further challenges in their personal and professional lives, reinforcing the interplay between mental health and running psychology.
Marathon Training Motivation: Keeping the Fire Alive
Marathon training requires significant dedication and can be mentally taxing. Maintaining motivation throughout the journey is vital for runners, and many employ various strategies to stay focused and driven. Goal-setting is a common technique used by marathoners; whether it’s improving personal bests, participating in fundraising, or simply finishing the race, these objectives provide a clear purpose and milestone for runners. Connecting with fellow participants also serves as a major motivating factor, creating mutual encouragement and support.
Additionally, understanding the deeper reasons behind why someone chooses to train for a marathon, especially an iconic race like the Boston Marathon, can fuel motivation. For many, the event is more than just a race—it’s a tribute to personal challenges, a means of honoring loved ones, and a catalyst for mental health advocacy. Knowing that their efforts can contribute to a greater cause often inspires runners to push past physical and mental barriers, reinforcing their commitment to the sport.
Reflections on the Boston Marathon Experience
The experience of participating in the Boston Marathon goes beyond mere competition; it’s a journey of self-discovery and reflection. Runners confront their limits, both physically and mentally, often leading to profound realizations about persistence and personal strength. As they approach the finish line, many participants grapple with emotions ranging from exhilaration to introspection. Each runner’s journey is unique, shaped by their background, mental fortitude, and reasons for running, making the event deeply personal.
The sense of achievement that comes from completing such a demanding race can transform a runner’s self-image. After the Boston Marathon, many individuals report feeling as though they’ve conquered not just the 26.2 miles but also significant emotional struggles in their lives. This transformation contributes to a greater understanding of how mental health and running intersect, further emphasizing the need for mental health conversations and support systems in distance running.
Harnessing Energy for Personal Growth
Harnessing the energetic force of marathon training and race day can lead to unimaginable personal growth. Many runners cite the Boston Marathon as a pivotal moment in their lives, where they can channel their challenges, fears, and triumphs into constructive energy. This concept of energy being channeled into a focused endeavor becomes fundamental during marathon training, promoting resilience and mental fortitude. The marathon becomes a metaphor for overcoming life’s challenges, serving as a powerful reminder of what they are capable of achieving.
Moreover, Brown’s insights into the emotional spectrum experienced by runners emphasize how this energy can unify them, creating a compelling bond. Participants share stories that fuel motivation and encourage mental toughness, strengthening their resolve. This shared experience of harnessing personal struggles into something visibly rewarding—a marathon medal—becomes a transformative moment for individuals, showcasing the psychological benefits of committing to such a significant endeavor.
The Role of Community in Running
Community support is a cornerstone of the marathon experience, especially during events like the Boston Marathon. The camaraderie fostered among runners provides emotional strength—knowing that others are on a similar journey can alleviate feelings of isolation. Training with a group or seeking encouragement from friends and family reinforces the motivation needed to keep pushing forward. This network transforms the solitary act of running into a shared experience, where mutual support enhances mental well-being.
In the larger context, the Boston Marathon brings together individuals from diverse backgrounds, each contributing to a unified goal. As runners cheer each other on, they foster a sense of belonging, which reinforces the positive psychological impact running has on mental health. Through this shared experience, participants not only enhance their individual training but also build an unbreakable bond over the challenge they collectively undertake, highlighting the powerful role of community within the sport.
Understanding Psychological Distress in Marathon Finishers
Across the finish line, emotional responses can vary significantly among marathon finishers. While some celebrate their hard-earned achievements, others may find themselves overwhelmed and in distress. The work of mental health professionals at events like the Boston Marathon is crucial in identifying these moments of acute psychological pain. Understanding the underlying factors that contribute to such distress is essential in providing effective mental health support for runners, ensuring they are cared for both physically and mentally.
The experiences shared by the Boston Marathon finishers encapsulate a broad spectrum of emotional responses. From celebrating moments of personal tribulation to grappling with feelings of failure or anxiety, all are valid experiences that deserve attention. The role of mental health support at marathon events, including post-race evaluations, is critical in fostering not only physical recovery but also mental clarity, allowing participants to reconcile their experiences.
The Transformational Power of Achievement in Running
Completing a marathon, and particularly the Boston Marathon, represents a significant achievement that goes beyond just crossing a finish line. For many, it marks the culmination of months of dedication, training, and mental preparation. This transformational moment can lead to increased confidence and a renewed sense of purpose. Runners often describe how the achievement of finishing a marathon boosts their self-esteem, proving to themselves that they can achieve difficult goals despite life’s obstacles.
The medal awarded at the finish serves as a tangible reminder of this accomplishment, reinforcing the connection between mind and body. Psychologist Jeff Brown highlights how these moments signify hope and fulfillment, bridging the gap between struggle and success. The profound emotional reactions witnessed at the finish line mirror the deep psychological impact that such achievements have on individuals—emphasizing the potent link between running, personal resolution, and mental health.
Integrating Mindfulness and Running for Mental Well-Being
Integrating mindfulness into running can significantly enhance mental well-being. Runners are often encouraged to focus on their breath, their steps, and the sensations of the moment rather than the finish line. This practice not only helps in relieving stress but also fosters a deeper connection between mind and body. Mindfulness in running encourages athletes to appreciate the journey, cultivate patience, and develop mental resilience—a vital trait when preparing for an extensive race like the Boston Marathon.
Many athletes find that incorporating mindfulness into their training routines can lead to improved race performance. When runners are present and focused, they can better manage their thoughts and emotions, which is crucial during the Boston Marathon’s rigors. This mental clarity not only boosts their confidence but also enhances their overall experience, proving that running can be as much about mental health and awareness as it is about physical endurance.
Frequently Asked Questions
How does Boston Marathon mental health support help runners during the race?
Boston Marathon mental health support plays a crucial role in attending to the emotional and psychological needs of runners. The support teams, including psychologists, are available to assess runners who may experience acute distress, confusion, or physical challenges during the race. This allows runners to receive immediate assistance, helping them cope with their feelings and ensuring their well-being is prioritized throughout the event.
What are the psychological benefits of running in the Boston Marathon?
The psychological benefits of running in the Boston Marathon are significant. Many finishers experience a boost in self-esteem and personal fulfillment as they conquer the 26.2 miles. The event also offers a unique opportunity for reflection, connection, and celebration of personal goals, which can lead to improved mental health and resilience as runners acknowledge their hard work and dedication.
What motivates runners in the Boston Marathon beyond physical fitness?
Many runners in the Boston Marathon are motivated by personal stories, such as running in memory of loved ones or raising funds for charities. This emotional connection adds depth to their training and perseverance during the race. Additionally, the prestigious nature of the Boston Marathon and the sense of community among participants inspires many to push their limits, highlighting the intertwining of personal journeys and mental health resilience.
Can marathon training help improve mental health for Boston Marathon participants?
Yes, marathon training can significantly enhance mental health for Boston Marathon participants. The structured training process encourages discipline, offers stress relief, and fosters a strong sense of achievement. As runners prepare for the race, they often experience reductions in anxiety and depression, alongside improvements in mood and self-perception, all of which contribute to better overall mental health.
What should runners know about the mental challenges they might face during the Boston Marathon?
Runners should be aware that mental challenges during the Boston Marathon can include fatigue, self-doubt, and the pressure of performing well. It’s crucial to prepare mentally as well as physically, using techniques such as visualization and positive self-talk. Understanding that encountering these feelings is normal can help runners manage their expectations and improve their resilience throughout the race.
How does the community aspect of the Boston Marathon impact mental health?
The community aspect of the Boston Marathon significantly enhances the mental health of participants. The support from spectators, fellow runners, and volunteers creates an encouraging environment. This sense of camaraderie not only motivates runners but also fosters a feeling of belonging and shared experience, which is vital for mental well-being during such a challenging event.
| Key Points | Details |
|---|---|
| Motivation to Run | Personal reasons vary greatly, from commemorating loved ones to personal health challenges. |
| Physical and Mental Challenges | Some runners face severe physical distress and require medical assistance after the marathon, showcasing the toll it takes on their bodies. |
| Transformational Experience | Completing the Boston Marathon is seen as a significant accomplishment, offering recognition and a sense of personal achievement. |
| Mental Health Support | The presence of mental health professionals is crucial to support runners facing emotional and psychological challenges during the marathon. |
| Public Perception | Finishing the marathon transforms how runners see themselves and how they are viewed by others, evoking a sense of heroism. |
Summary
Boston Marathon mental health is prominently highlighted through the experiences and challenges faced by runners. Many participate for deeply personal reasons, but the journey often stretches beyond physical endurance to encompass significant mental health aspects. The support from mental health professionals is essential in managing the emotional distress that can arise during and after the race. Ultimately, running the Boston Marathon is not only a test of physical strength but also a powerful journey of self-discovery and affirmation that resonates with countless individuals.
TIM-3 Therapy for Alzheimer’s: A New Hope for Patients
TIM-3 therapy for Alzheimer’s emerges as a groundbreaking approach in the fight against this debilitating disease, offering new hope for effective Alzheimer’s treatment. A recent study has shown that inhibiting the TIM-3 checkpoint molecule can revitalize the brain’s immune cells, known as microglia, enabling them to effectively combat Alzheimer’s plaques and restore memory function in animal models. By turning off this inhibitory pathway, researchers have demonstrated improved cognitive abilities, paving the way for potential applications in human patients. This innovative strategy not only sheds light on the role of the immune system in Alzheimer’s but also draws parallels with successful cancer therapies that utilize similar mechanisms. As research progresses, TIM-3 therapy could redefine how we understand and treat Alzheimer’s disease, potentially transforming the lives of millions affected by cognitive decline.
New advancements in Alzheimer’s therapy, particularly the TIM-3 strategy, represent a shift in how we perceive immune interactions within the brain. Known for its role in regulating immune responses, TIM-3 could be key to unlocking effective treatments for Alzheimer’s disease. By targeting this checkpoint molecule, we can enhance the brain’s innate immune response, allowing microglia to clear harmful amyloid plaques that hinder cognitive function. The intersection of cancer research and neurodegenerative disease treatments paves an exciting avenue to explore immune system modulation as a viable option in addressing conditions like Alzheimer’s. As we delve deeper into the implications of TIM-3 modulation, the potential for innovative solutions in Alzheimer’s management becomes increasingly promising.
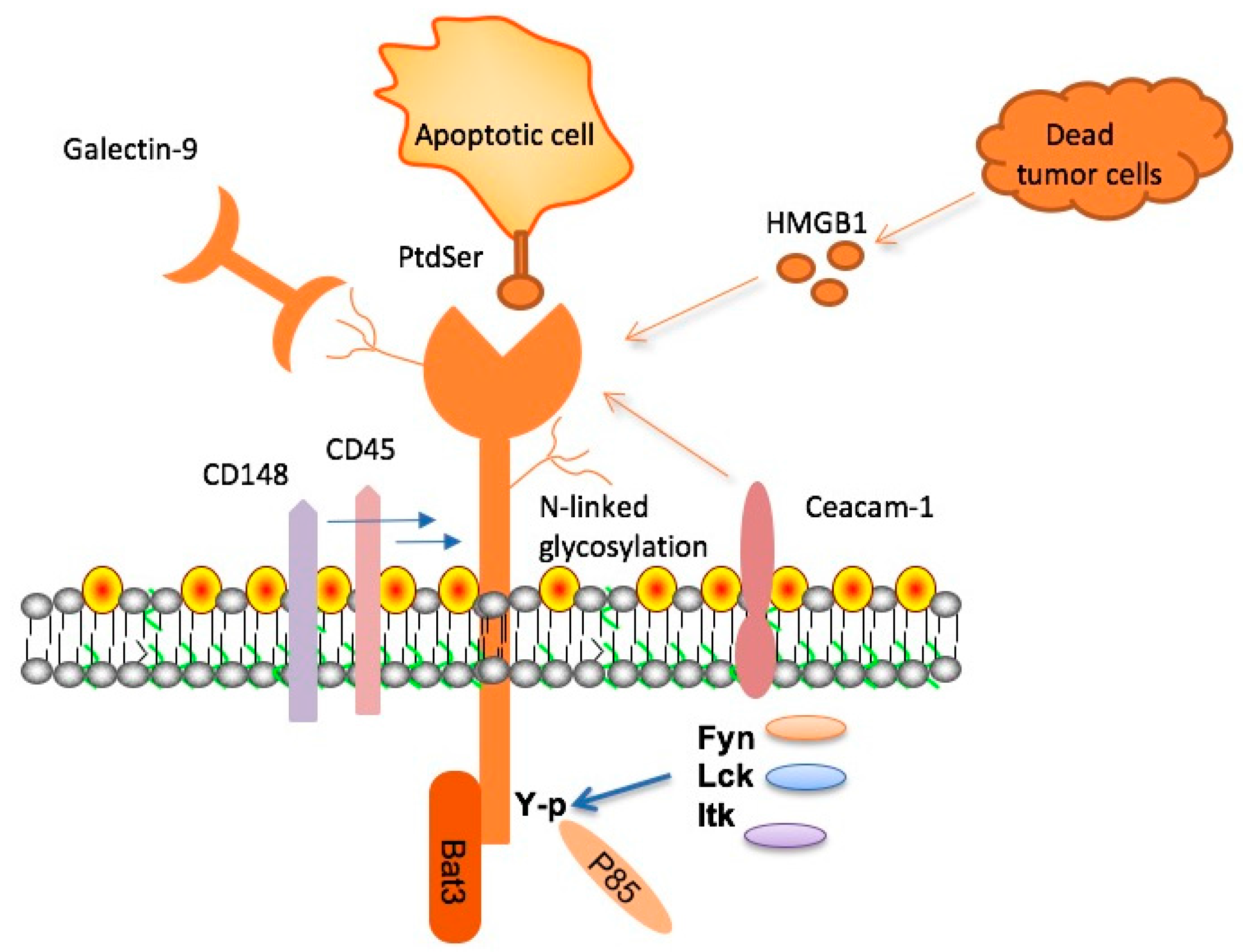
The Role of TIM-3 in Alzheimer’s Disease
TIM-3, or T-cell immunoglobulin mucin-3, is an inhibitory molecule that plays a crucial role in the immune system’s regulation. In the context of Alzheimer’s disease (AD), TIM-3 has been identified as a significant factor that hinders microglia, the brain’s immune cells, from efficiently clearing harmful amyloid plaques. These plaques contribute to cognitive decline and memory loss in individuals with Alzheimer’s. The connection between TIM-3 and late-onset Alzheimer’s disease suggests it could serve as a critical target for therapeutic interventions aimed at enhancing immune responses against these damaging proteins in the brain.
In lab studies, when TIM-3 expression was inhibited in genetically modified mice, researchers observed remarkable changes in plaque management. Microglia were able to engage and clear amyloid plaques more effectively, which not only reduced plaque size but also improved cognitive functions in these animals. This finding highlights the potential of TIM-3-targeted therapies as a groundbreaking approach to treating Alzheimer’s disease by leveraging the body’s immune system to combat the condition.
TIM-3 Therapy: A Potential Breakthrough for Alzheimer’s Treatment
Research into TIM-3 therapy for Alzheimer’s shows promising potential as it borrows from successful cancer treatment strategies. By blocking the inhibitory effects of TIM-3 on microglia, this therapy aims to restore the immune system’s ability to clear amyloid plaques from the brain. Anti-TIM-3 antibodies or small molecules could be administered to Alzheimer’s patients to activate microglia effectively, allowing them to respond to and eliminate plaques that contribute to the disease’s progression.
This concept builds on the understanding that inhibiting checkpoint molecules like TIM-3 has already yielded benefits in cancer immunotherapy. If successfully translated to Alzheimer’s treatment, TIM-3 therapy could halt or even reverse the cognitive decline associated with the disease. Early studies indicate that such therapies could be less likely to lead to vascular damage compared to existing anti-amyloid treatments, as TIM-3 selectively targets the microglial response rather than circulating antibodies affecting brain endothelial cells.
Understanding Microglia: The Immune Cells of the Brain
Microglia serve as the brain’s primary immune cells, constantly on alert to maintain a healthy environment by pruning synapses and clearing debris. As individuals age, however, the function of microglia can diminish, with increased TIM-3 expression causing them to become homeostatic. This shift leads to reduced efficacy in clearing amyloid beta plaques and can contribute to the development of Alzheimer’s disease. Understanding the role of microglia in synaptic health and their response to parental aging is essential for identifying potential therapeutic targets for AD.
In Alzheimer’s patients, it’s observed that microglia express significantly higher levels of TIM-3, reflecting a dysfunctional state where they fail to actively engage with and eliminate pathological amyloid plaques. This impairment suggests that interventions aimed at decreasing TIM-3 expression could restore the natural phagocytic function of microglia, allowing them to clear plaques and potentially alleviate memory impairments associated with the disease.
The Genetic Link Between TIM-3 and Late-Onset Alzheimer’s
The connection between TIM-3 and late-onset Alzheimer’s disease has been substantiated by genome-wide association studies that identify TIM-3, or HAVCR2, as a genetic risk factor. This polymorphism indicates that individuals with specific variations in the TIM-3 gene may exhibit a heightened susceptibility to developing Alzheimer’s as they age. The molecular mechanisms behind this link reveal that TIM-3’s role as a checkpoint molecule not only affects immune responses but is also critical in maintaining cognitive health.
Moreover, the presence of TIM-3 on microglia in Alzheimer’s patients provides a potential target for new treatments. By focusing on individuals with this specific genetic predisposition, scientists can tailor therapies that counteract the harmful effects of TIM-3, thereby enhancing the brain’s innate ability to clear harmful plaques and protect cognitive function in the aging population.
Current Research and Future Perspectives on TIM-3 Therapy
Recent studies exploring TIM-3 therapy for Alzheimer’s disease highlight the need for innovative approaches after several unsuccessful drug trials in the past. Research teams, including those from Harvard Medical School, are investigating the use of TIM-3 inhibitors to enhance microglial activity in Alzheimer’s mouse models. By observing the behavioral improvements in these models, researchers aim to gather compelling evidence of the potential benefits of targeting TIM-3 in human subjects with Alzheimer’s.
The future of TIM-3 therapy involves using genetically modified mouse models that incorporate the human TIM-3 gene, leading to more accurate preclinical testing for therapies available to humans. As exciting discoveries emerge, there may be pathways leading to the development of new, effective treatments that harness the body’s immune system, paving the way for enhanced management of Alzheimer’s disease and a comprehensive strategy to combat its debilitating effects on memory and cognition.
Challenges in Alzheimer’s Disease Treatment and TIM-3 Potentials
Despite progress made in Alzheimer’s research, numerous challenges remain in developing effective therapies. Conventional anti-amyloid treatments have shown limited success, often failing to demonstrate significant cognitive benefits while presenting risks of vascular complications. This positions TIM-3 therapy as a unique opportunity to re-evaluate treatment strategies, emphasizing the importance of harnessing the immune system’s potential without the associated side effects of existing treatments.
The versatility of TIM-3-targeting strategies could provide a much-needed alternative for Alzheimer’s treatment. By focusing on the disease’s underlying biology and the role of microglia, there’s hope that TIM-3 therapy can not only mitigate plaque accumulation but also enhance cognitive function significantly, transforming the landscape of Alzheimer’s disease management.
The Mechanism of Immune System Activation in Alzheimer’s Therapy
One of the most exciting aspects of TIM-3 therapy is its mechanism of action. By disabling the inhibitory signals sent by TIM-3, microglia are empowered to engage actively with amyloid plaques, promoting their clearance and allowing cognitive functions to recover. This shift represents a significant departure from traditional models of treatment that focus solely on reducing plaque burden, showcasing a holistic approach that involves reinstating the immune system’s natural capabilities.
Activating the immune system through TIM-3 inhibition not only targets plaque-related pathology but also aims to rejuvenate the overall health of the brain. This dual benefit could help slow the progression of Alzheimer’s disease while concurrently restoring some degree of normal memory function, an appealing prospect for both patients and researchers alike.
Collaborative Efforts in Alzheimer’s Research and TIM-3 Development
The multidisciplinary approach to Alzheimer’s research is essential for rapidly transitioning discoveries into clinical applications. The collaboration between experts in neurology, immunology, and genetics underscores the importance of diverse perspectives in the exploration of TIM-3 therapy for Alzheimer’s. Combining expertise allows for an innovative framework that addresses the multifaceted nature of Alzheimer’s disease and effectively targets both immune dysfunction and pathogenic processes.
Involving institutions, researchers, and funding bodies further enhances the pace at which advancements can be achieved. Shared resources and knowledge enable quicker analysis of TIM-3’s role in Alzheimer’s, optimizing the development and testing of potential therapies. Through collective effort and dedication, the outlook for combating Alzheimer’s disease through TIM-3 therapy can become a reality.
Alzheimer’s Treatment Landscape: Integrating TIM-3 Insights
The landscape of Alzheimer’s treatment continues to evolve with insights gained from TIM-3 studies alongside other therapeutic avenues. By synthesizing findings from immune system research and traditional Alzheimer’s treatments, a more comprehensive strategy can emerge to offer holistic solutions for patients battling this complex disease. TIM-3 therapy presents an innovative angle that could realign existing treatment paradigms, emphasizing the immune response as a critical component of effective therapy.
Incorporating TIM-3 findings with ongoing research in other areas of Alzheimer’s treatment, such as the neuroinflammatory response and tau pathology, could pave the way for combination approaches that enhance patient outcomes. Ultimately, integrating TIM-3 insights with broader therapeutic strategies holds the potential for developing more effective, targeted treatments that may significantly improve the quality of life for those affected by Alzheimer’s disease.
Frequently Asked Questions
What is TIM-3 therapy for Alzheimer’s and how does it work?
TIM-3 therapy for Alzheimer’s leverages the inhibition of the TIM-3 checkpoint molecule, which restricts the activity of microglia—immune cells in the brain. Recent studies show that blocking TIM-3 allows microglia to clear amyloid plaques, leading to improved cognitive function. This approach transforms the TIM-3 pathway, which is typically exploited in cancer therapy, to enhance the immune response against Alzheimer’s plaques.
How is TIM-3 related to the immune system in Alzheimer’s treatment?
TIM-3 is a checkpoint protein that regulates immune responses, including those in Alzheimer’s disease. It inhibits microglia from attacking harmful amyloid plaques in the brain, leading to cognitive decline. By targeting TIM-3, therapeutic strategies aim to boost microglial activity, allowing these immune cells to effectively clear plaques and potentially restore memory functions.
Can TIM-3 therapy for Alzheimer’s benefit those with late-onset Alzheimer’s?
Yes, TIM-3 therapy holds promise for treating late-onset Alzheimer’s, which accounts for the majority of cases. Research indicates a genetic link between TIM-3 expression and late-onset Alzheimer’s, suggesting that therapies targeting this checkpoint molecule may help alleviate symptoms by enhancing microglial plaque clearance.
What are the potential side effects of TIM-3 therapy for Alzheimer’s patients?
While TIM-3 therapy for Alzheimer’s is still in experimental stages, potential side effects may include alterations in immune function due to the modulation of microglial behavior. Close monitoring will be necessary to ensure that enhancing microglial activity does not lead to unintended consequences, such as increased inflammation.
How does the deletion of TIM-3 gene in mice demonstrate the therapy’s effectiveness?
In studies where the TIM-3 gene was deleted in mice, researchers found that microglia could effectively remove amyloid plaques from the brain. This therapeutic model shows improved memory and cognitive function, highlighting that removing the inhibitory effects of TIM-3 can significantly benefit Alzheimer’s treatment and provide insights for human applications.
What research supports the use of TIM-3 therapy in Alzheimer’s plaques treatment?
Recent research published in high-impact journals has demonstrated that TIM-3 plays a critical role in inhibiting microglial clearance of amyloid plaques. By inhibiting TIM-3 in mouse models of Alzheimer’s, researchers observed cognitive improvement and better plaque management, paving the way for future clinical applications of TIM-3 therapy in Alzheimer’s treatment.
Is TIM-3 therapy being tested in human trials for Alzheimer’s?
Currently, TIM-3 therapy is in the preclinical stage, focusing on mouse models. However, the transition to human trials is a goal, as researchers are modifying models to test anti-TIM-3 antibodies for their potential efficacy in halting plaque development in patients with Alzheimer’s. Future studies will be crucial to validate these findings in humans.
| Key Points |
|---|
| Research indicates that TIM-3 therapy may improve cognitive function in Alzheimer’s patients by enabling microglia to attack amyloid plaques. |
| TIM-3 is an immune checkpoint molecule that inhibits microglia from clearing plaques. |
| Genetic polymorphisms in the TIM-3 gene increase the risk of late-onset Alzheimer’s disease. |
| The study was a collaboration involving multiple researchers over a five-year period, showing significant progress in Alzheimer’s therapy. |
| Removing TIM-3 expression in mice led to improved memory and reduced plaque accumulation in the brain. |
| Future treatments may involve the use of antibodies or small molecules to inhibit TIM-3 activity in humans. |
Summary
TIM-3 therapy for Alzheimer’s presents a promising avenue for treating this devastating disease. Recent research highlights the role of TIM-3, a checkpoint molecule that inhibits the brain’s immune cells, preventing them from clearing harmful amyloid plaques. By deleting TIM-3, studies in mouse models have shown improvements in memory and cognitive function. This innovative approach, which repurposes existing TIM-3 antibodies, offers hope in the fight against Alzheimer’s disease and could lead to significant advancements in therapeutic strategies.

Hemophilia B Treatment: New Advances in Gene Therapy
Hemophilia B treatment represents a significant leap forward in managing this often debilitating condition, particularly with the advent of innovative therapies like Hemgenix. This groundbreaking gene therapy not only alleviates the need for frequent injections but potentially provides long-term relief for those living with hemophilia. By harnessing recent advancements in gene therapy, patients now have the opportunity to experience a remarkable transformation in their quality of life. Moreover, the promise of gene therapy for hemophilia has invigorated medical research and patient hope, suggesting a future where painful bleeds become a thing of the past. With each new development, we move closer to a world where hemophilia B treatment becomes synonymous with healing and empowerment.
The treatment options for individuals with hemophilia B have evolved significantly over the years, particularly with the introduction of advanced therapies that leverage genetic engineering. These alternative approaches, often grouped under the umbrella of gene therapy, are reshaping how patients manage their condition and their expectations for the future. Many individuals suffering from this disorder are discovering the potential of being free from the burden of constant factor IX injections. As the scientific community continues to explore the potential of gene therapy advancements, patients can look forward to transformative solutions that address not just the symptoms, but the underlying causes of hemophilia. Ultimately, these developments signify a vital shift in the conversation about living with hemophilia, moving towards a more hopeful and empowered patient experience.
Understanding Hemophilia B and Its Impact
Hemophilia B is a genetic disorder that primarily affects males and results from a deficiency of factor IX, a crucial blood clotting protein. This condition can lead to spontaneous bleeding episodes, making even minor injuries potentially serious. It’s essential for individuals diagnosed with hemophilia B to manage their condition diligently, as untreated bleeds can lead to severe complications, including joint damage and other long-term health issues. Understanding the mechanisms of hemophilia B and its symptoms is vital for both patients and caregivers, ensuring timely interventions and appropriate treatments.
Living with hemophilia B requires a lifestyle that prioritizes safety and health management. Regular visits to healthcare providers for clotting factor treatments, along with lifestyle modifications to avoid injuries, are common. Patients often report feelings of isolation due to the limitations placed on their activities. However, advancements in treatment, including gene therapy, offer new hope for increased mobility and reduced fear of spontaneous bleeding. As technology evolves, so do the strategies for living a fulfilling life with hemophilia, emphasizing the importance of community and support.
Latest Advancements in Hemophilia B Treatment
The introduction of gene therapy for hemophilia B marks a pivotal moment in treatment strategies. One notable example is Hemgenix, a revolutionary therapy designed to correct the genetic defect causing hemophilia B. Approved by the FDA in late 2022, this treatment aims to provide long-lasting solutions that could potentially alleviate the need for frequent clotting factor injections. Patients undergoing this therapy can expect to experience a significant decrease in bleeding episodes, promoting a better quality of life and reducing the physical and emotional burden associated with the disorder.
Gene therapy advancements, such as Hemgenix, utilize targeted techniques to introduce a corrected version of the factor IX gene directly into the patient’s liver cells. This innovative method not only addresses the root cause of hemophilia B but also reduces the need for ongoing treatment, offering a semblance of normalcy to those affected by this condition. As research continues, further enhancements in hemophilia B gene therapy could lead to even more effective solutions, paving the way for a brighter future for patients globally.
Living with Hemophilia: Challenges and Triumphs
For individuals living with hemophilia B, daily life can involve unique challenges that affect physical health and emotional well-being. Managing routine activities often requires meticulous planning to avoid injuries that could lead to serious bleeding episodes. Social interactions can also become challenging, as many patients feel the need to educate their friends and family about their condition to ensure safe participation in activities. Despite these hurdles, many individuals develop resilience and find ways to engage fully in their communities and hobbies.
Despite the challenges, many patients report significant triumphs in living with hemophilia B. Sports, arts, and other creative outlets provide opportunities for self-expression and community connection. Moreover, support systems, including hemophilia advocacy groups and families, can play an instrumental role in helping individuals navigate their condition. The advancements in treatments through therapies like Hemgenix give hope for a future with fewer restrictions, equipping patients with the tools necessary to lead healthy and fulfilling lives.
The Role of Gene Therapy in Treating Hemophilia B
Gene therapy is reshaping the landscape of hemophilia B treatment by offering a potential long-term solution to a life-long condition. This innovative approach works by directly addressing the genetic cause of hemophilia B, providing patients with a new lease on life. Hemgenix, for example, aims to restore normal coagulation function through a one-time treatment, fundamentally changing how this bleeding disorder is managed. Patients can dream of a life free from routine factor infusions, as studies show that many who receive this therapy experience sustained therapeutic effects long after treatment.
Moreover, advancements in gene therapy are not just about treating the symptoms but attempting to cure hemophilia B at its source. This paradigm shift is welcomed by both patients and healthcare professionals who have witnessed the limitations of traditional treatments. With ongoing research and positive clinical trial results, the future of hemophilia B care looks promising, potentially unlocking new therapeutic avenues that could benefit countless individuals suffering from this challenging condition.
Understanding Gene Therapy Advancements
Recent advancements in gene therapy are revolutionizing the treatment landscape for various genetic disorders, including hemophilia B. These innovations focus on delivering therapeutic genes into patients’ cells to correct underlying genetic defects. The progress in this field, particularly with therapies like Hemgenix, illustrates a growing understanding of how best to approach complex genetic conditions. As scientists continue to refine techniques, the goal is to enhance safety and efficacy, making treatments more accessible for patients in need.
Gene therapy advancements not only promise to improve clinical outcomes but also aim to reduce treatment burdens for patients. With the potential to replace long-term, chronic treatment regimens with single-dose therapies, there is an increasing interest in this cutting-edge approach. Researchers are optimistic that continued exploration of gene therapies will lead to effective treatments for more diseases, providing hope for patients and families affected by a myriad of genetic disorders.
Market Challenges Facing Gene Therapies
Despite the promise of gene therapies like Hemgenix, significant challenges remain in balancing the economic realities of development with patient access to treatment. The high costs associated with these innovative therapies raise concerns about insurance coverage, access, and the sustainability of treatment options for patients. For many, the potential life-changing benefits of gene therapy may be overshadowed by financial hurdles, creating a disparity in who can receive these transformative treatments.
The future of gene therapies depends not only on scientific advancements but also on navigating the complexities of healthcare economics. As treatments for hemophilia B and other conditions continue to emerge, the industry must foster an environment where innovative therapies can thrive while remaining accessible to the patients who need them most. Collaboration among researchers, healthcare professionals, insurers, and advocacy groups is crucial to bridging the gap between groundbreaking science and practical patient care.
The Importance of Research and Development in Hemophilia Treatment
Research and development are the backbone of advancements in hemophilia treatment. As scientists investigate the genetic underpinnings of conditions like hemophilia B, they open the door to groundbreaking therapies that can potentially reduce or eliminate symptoms. Continuous R&D is necessary to ensure that new treatments, such as gene therapies, evolve with safety, efficacy, and patient needs at the forefront. Investing in hemophilia research enhances the prospect of finding not just better treatments but also potential cures.
Moreover, the translation of research findings to clinical practice is crucial in ensuring that patients benefit from the latest innovations. Collaborative efforts among academic institutions, biopharmaceutical companies, and healthcare providers contribute to a deeper understanding of hemophilia and pave the way for improved therapies. The hope is that ongoing commitment to research will lead to better outcomes for individuals living with hemophilia, transforming lives through more effective treatment options.
Social Impacts of Living with Hemophilia B
Living with hemophilia B can significantly impact social interactions and relationships. Many individuals grapple with embarrassment or shame related to their condition, leading them to withdraw from activities or avoid social settings altogether. It’s essential for patients to have support systems in place, whether through family, friends, or support groups, to help navigate these emotional challenges. Encouraging open conversations about hemophilia can promote understanding and acceptance among peers, alleviating some of the social burdens patients face.
In addition to personal relationships, the broader societal impact of hemophilia B cannot be overlooked. Education and awareness initiatives about hemophilia are necessary to foster a more inclusive understanding of the condition. By informing communities and eliminating stigma, individuals living with hemophilia can feel more empowered to participate in everyday activities and advocate for their health needs. As more people become knowledgeable about hemophilia, the hope is for a culture of acceptance and support that enhances the quality of life for those affected.
Looking Forward: The Future of Hemophilia B Treatments
As we look towards the future, the landscape of hemophilia B treatment is poised for significant change. With emerging gene therapies like Hemgenix offering promising results, the medical community remains hopeful for a time when these advancements will fully integrate into standard practices. The ongoing dedication to research and development is critical in overcoming the remaining challenges, ensuring that treatment becomes even more effective and widely available.
The journey toward eliminating the burdens of hemophilia B is not just about medical innovation; it’s also about transforming patient experiences and outcomes. As authorized therapies are developed and refined, the potential for improved quality of life becomes a tangible reality for individuals living with hemophilia B. Collaboration among stakeholders—from researchers to patients and healthcare providers—will be key to realizing this vision of a future where hemophilia is manageable and possibly curable.
Frequently Asked Questions
What are the latest advancements in hemophilia B treatment with gene therapy?
Recent advancements in hemophilia B treatment include the introduction of gene therapies like Hemgenix. This innovative therapy targets the liver and aims to correct the genetic mutation responsible for hemophilia B, potentially reducing the need for regular factor IX injections and helping patients live more normal lives.
How does Hemgenix treatment work for hemophilia B?
Hemgenix treatment for hemophilia B utilizes a viral vector to deliver a corrected copy of the gene responsible for producing coagulation factor IX directly into the liver. This process encourages the body to produce its own clotting factor, stabilizing patients and significantly improving their quality of life.
What is gene therapy’s impact on living with hemophilia B?
Gene therapy, particularly treatments like Hemgenix, has the potential to transform the experience of living with hemophilia B. By correcting the underlying genetic issue, patients may achieve stable factor levels, reduce or eliminate the need for regular infusions, and enjoy a more active, worry-free lifestyle.
Are there any risks associated with gene therapy for hemophilia B?
While gene therapy for hemophilia B, such as Hemgenix, shows immense promise, there are potential risks involved, including immune responses to the viral vector and the new gene, as well as unknown long-term effects. Patients should discuss these risks with their healthcare providers before proceeding with treatment.
What is the cost of gene therapy for hemophilia B like Hemgenix?
The cost of Hemgenix, a gene therapy for hemophilia B, is approximately $3.5 million, though negotiated rates with insurance companies can lower this figure. Understanding the financial implications and discussing insurance coverage is crucial for patients considering this treatment option.
How does Hemgenix improve the lives of hemophilia B patients?
Hemgenix significantly improves the lives of hemophilia B patients by potentially eliminating the need for frequent factor IX treatments. Many patients experience increased factor levels, allowing for greater physical activity and reducing the anxiety associated with bleeding episodes.
What should patients expect during the hemophilia B gene therapy treatment process?
Patients receiving gene therapy for hemophilia B can expect a relatively straightforward outpatient procedure. The treatment involves a short infusion process, and many report minimal side effects, allowing them to return to their daily activities soon after.
How does gene therapy for hemophilia B compare to traditional treatments?
Gene therapy for hemophilia B offers a fundamentally different approach compared to traditional treatments, which typically involve regular factor IX injections. Gene therapy aims to provide a long-term solution by correcting the genetic cause of the condition, potentially leading to significant reductions in treatment frequency and associated healthcare costs.
| Key Point | Details |
|---|---|
| Introduction to Terence Blue | Terence Blue, diagnosed with hemophilia B at a very young age, received gene therapy at Brigham and Women’s Hospital. |
| Gene Therapy – Hemgenix | Developed by CSL Behring and approved by FDA in 2022, it aims to provide long-lasting benefits with a single treatment. |
| Treatment Costs | Costing approximately $3.5 million, insurance negotiations can lower prices but market pressures remain a challenge. |
| Patient Experience | Blue’s treatment marks a significant change, as he has experienced quicker healing and less reliance on clotting factor injections. |
| Future of Gene Therapies | Despite high costs and market challenges, gene therapies for hemophilia and other conditions are expanding, with optimism for effective treatments. |
Summary
Hemophilia B treatment has taken a significant step forward with the introduction of gene therapy like Hemgenix, providing hope for individuals who have long managed the condition through regular injections. Terence Blue’s experience demonstrates the potential for transformative outcomes, including reduced reliance on traditional treatments and improved healing rates. As the landscape of gene therapies continues to evolve, the focus remains on balancing innovation with cost and patient accessibility to ensure that more people can benefit from these advancements.

Shared Meals and Happiness: Key to Well-Being
Shared meals and happiness are intertwined in ways that extend beyond mere nourishment. Studies suggest that the act of dining together significantly enhances life satisfaction, revealing a crucial connection between social interaction and emotional well-being. Recent happiness research emphasizes that consistency in mealtime companionship can be more telling of one’s overall happiness than traditional markers like income or employment status. As Americans increasingly dine alone, with alarming statistics showing one in four opting for solitary meals, the importance of shared meals has never been clearer. Encouraging social connections through meal sharing not only offsets the rising trend of solitary dining but also taps into the numerous meal sharing benefits for mental health and community ties.
Meal times serve as more than just periods for eating; they become vital gatherings that can nurture relationships and boost well-being. The concept of communal dining encompasses the social aspects of sharing food, which has been highlighted as an important factor for personal contentment across various cultures and age groups. As research shows, those who frequently engage in shared dining experiences often report higher levels of joy and connection, making it a fundamental aspect of human interaction. With the significant increase in statistics showing lonely dining habits, fostering environments for collective meals could be a crucial step towards revitalizing social bonds and enhancing overall happiness. Exploring alternative avenues to elevate communal dining practices can lead to profound benefits for individuals and communities alike.
The Importance of Shared Meals in Fostering Happiness
Shared meals have been shown to significantly impact emotional well-being, highlighting the crucial role they play in cultivating happiness. Research suggests that communal dining is not merely a cultural practice but a vital contributor to one’s overall sense of satisfaction in life. By enjoying food with friends or family, individuals can forge deeper social connections, which are essential for mental health. The joy of laughter and conversation around a table creates a supportive environment that fosters positive emotions; thus, engaging in shared meals is more than just a pleasurable experience—it’s a pathway to increased well-being.
Furthermore, the act of sharing food transcends mere nourishment; it’s also about bonding and community. Studies indicate that adults who frequently dine with others tend to report higher levels of happiness than those who dine alone. This phenomenon is particularly critical in light of the alarming statistics regarding dining alone—where a staggering 1 in 4 Americans now report eating all meals in solitude. These findings reinforce the idea that our dining habits directly influence our emotional health and advocate for a cultural shift towards more communal experiences to enhance our quality of life.
Dining Alone: A Growing Trend and Its Implications
Recent statistics reveal a concerning trend in American society: the increase in individuals dining alone. According to the American Time Use Survey, there has been a staggering 53% rise in those who reported eating all their meals alone since 2003. This trend cuts across all demographics, but particularly impacts younger individuals. Such solitary meals represent a significant shift in social behavior that may be linked to the deterioration of social connections, which are crucial for emotional support and resilience in the face of life’s challenges.
The implications of this growing trend are profound. Dining alone not only deprives individuals of the happiness associated with shared meals but may also lead to increased feelings of isolation and loneliness. As research continues to emerge on happiness and social interactions, it’s clear that reconnecting with family and friends over meals could play an essential role in reversing this trend. Encouraging communal dining experiences might not only enhance individual well-being but also contribute to a healthier, more engaged society.
Exploring Meal Sharing Benefits
The benefits of sharing meals extend beyond just enhancing happiness; they also contribute positively to our physical health and cognitive function. Meal sharing encourages individuals to partake in a variety of foods, often leading to healthier dietary choices and improved nutrition. For instance, when eating with others, individuals are more likely to choose balanced meals, incorporating fruits and vegetables, which are vital for maintaining health and reducing the risk of chronic diseases. Therefore, promoting shared meals can have far-reaching effects on public health.
Additionally, the act of shared dining stimulates conversation and social discourse, aiding cognitive development and strengthening memory through meaningful interactions. Parents who regularly share meals with their children are likely to instill communication skills and promote emotional intelligence, setting a foundation for future social interactions. In essence, the benefits of meal sharing reach far beyond the dining table; they have the potential to transform both personal and public health landscapes.
Social Connections and Their Role in Well-Being
Social connections play an essential role in our happiness and overall well-being. Research has frequently shown that strong relationships contribute to greater happiness and life satisfaction. Regular interactions, particularly during shared meals, can enhance feelings of belonging and community, which are fundamental to human happiness. As personal and social challenges mount in today’s world, fostering strong social ties becomes increasingly important in managing stress and promoting resilience.
The evidence supporting the link between social connections and well-being underscores the need for community-building efforts that encourage communal dining experiences. Community organizations and local governments can play a vital role in facilitating events that bring people together around food. By creating opportunities for shared meals, we can help combat the loneliness epidemic and cultivate a supportive community atmosphere that contributes to a healthier society overall.
Happiness Research: Insights into Meal Sharing
Understanding the relationship between happiness and meal sharing has become a focal point for researchers seeking insights into human behavior. Studies show that sharing meals is a powerful predictor of happiness across various demographics, suggesting that how we eat influences our emotional and psychological health. Utilizing methodologies that assess both subjective measures of happiness and objective indicators, researchers aim to unpack the complexities of this budding field, with meal sharing emerging as a potential focal point for intervention and policy.
As scholars delve into happiness research, the correlations between social interactions during meals and emotional well-being continue to grow clearer. Discussions surrounding the psychological benefits of social dining experiences can inform public health strategies aimed at reducing loneliness and enhancing social cohesion. Ultimately, ongoing research will provide further insight into how meal sharing can be leveraged as a tool for improving overall life satisfaction across diverse populations.
Creating Awareness Around the Benefits of Communal Dining
Raising awareness about the significance of communal dining is essential in reversing trends of isolation and loneliness. By highlighting the benefits of shared meals, families, friends, and communities can be encouraged to prioritize meal times together. Educating the public about the profound impact communal eating has on happiness can motivate individuals to reconnect with loved ones, enhancing emotional wellbeing while simultaneously building stronger community ties.
Awareness campaigns can be implemented at various levels, from schools promoting family meals to local organizations hosting community dinners. By cultivating an environment where shared meals are celebrated and valued, we can enhance not only individual happiness but also foster a sense of belonging. Ultimately, such initiatives can lead to a more connected and vibrant society, proving that the simple act of sharing a meal holds the power to transform lives.
Interventions for Increasing Shared Meals
To address the challenges posed by increasing dining alone statistics, it is crucial to develop and implement interventions that promote shared meals. Initiatives such as community potlucks, group cooking classes, and dining events can create opportunities for interaction and relationship-building. By encouraging individuals to come together over food, these interventions can help reduce isolation while enhancing social connections, which are vital for happiness.
Moreover, policymakers can play a significant role in supporting these initiatives by providing resources or incentives for community-building activities centered around meals. Schools and workplaces can also contribute by implementing programs that encourage group meals. By emphasizing the importance of spending time together over meals, we can foster a culture that values connection and community, ultimately leading to happier, healthier individuals.
The Cultural Significance of Shared Meals
Shared meals are deeply rooted in cultural traditions around the globe, often representing more than just sustenance; they embody values of community and togetherness. Across various cultures, dining together is a ritual that strengthens family bonds, fosters friendships, and facilitates the sharing of stories, reinforcing social ties and cultural heritage. Understanding the cultural significance of shared meals can encourage societies to uphold these practices amidst modern pressures that encourage individualism and isolation.
Furthermore, emphasizing the cultural aspects of communal dining can create a sense of pride and belonging among individuals. It allows people to connect with their heritage while reinforcing the importance of sharing moments over food. By celebrating the cultural traditions associated with meal sharing, societies can work towards creating inclusive environments where communal dining becomes an integral part of daily life, promoting happiness and social connection for all.
Future Research Directions: Meal Sharing and Happiness
The exploration of the nexus between meal sharing and happiness continues to evolve, with future research expected to provide deeper insights into this relationship. Researchers are keen to investigate the causal dynamics at play—whether sharing meals actively contributes to happiness or if happier individuals naturally tend to share meals more frequently. This duality highlights the necessity for complex studies that can parse these variables, providing clearer pathways for interventions focusing on social eating.
Moreover, the impact of cultural and contextual factors on meal sharing and happiness also deserves attention. By comparing diverse populations, researchers can identify universal trends and customize interventions that resonate with specific communities. As the body of knowledge in this area grows, it is likely that practical applications will emerge, providing targeted solutions for enhancing communal dining and thus improving overall happiness and well-being within society.
Frequently Asked Questions
What is the importance of shared meals in relation to happiness?
Shared meals are crucial for happiness as they foster positive social connections and enhance emotional well-being. Research shows that individuals who enjoy more meals with others report higher satisfaction in life, making meal sharing a vital component of overall happiness.
How do shared meals contribute to social connections and emotional well-being?
Meal sharing promotes social connections by bringing people together, which can lead to stronger relationships and a greater sense of community. These social interactions are linked to increased positive emotions, highlighting the importance of shared meals in enhancing emotional well-being.
Are dining alone statistics indicative of happiness levels?
Yes, dining alone statistics reveal a concerning trend that can be linked to lower happiness levels. As studies indicate, an increasing number of individuals report eating alone, which correlates with decreased life satisfaction and emotional well-being.
What are the benefits of meal sharing for mental health?
The benefits of meal sharing for mental health include reduced feelings of loneliness, improved mood, and enhanced social support systems. Shared meals create a sense of belonging, which is essential for maintaining high levels of happiness and mental well-being.
Does happiness research support the idea that meal sharing improves well-being?
Yes, happiness research strongly supports that meal sharing significantly improves well-being. Studies have found that individuals who frequently dine with others experience greater life satisfaction and improved emotional health, indicating a clear link between shared meals and happiness.
How can we encourage more meal sharing in today’s society?
Encouraging more meal sharing can be achieved through community programs, social clubs, and family initiatives that highlight the importance of shared dining experiences. By promoting these interactions, we can improve social connections and overall well-being.
Is there a relationship between shared meals and the societal trend of dining alone?
Yes, there is a relationship where an increase in dining alone correlates with a decline in overall happiness and social satisfaction. As more individuals eat alone, the opportunity for shared meals, which enhance happiness, decreases, potentially impacting mental health.
What are the proposed policy interventions related to shared meals and happiness?
Proposed policy interventions could include community dining initiatives, funding for shared meal programs, and campaigns promoting the benefits of eating together, all aimed at improving social cohesion and enhancing overall public happiness.
| Key Points | Details |
|---|---|
| Shared Meals and Happiness | Dining with others is linked to higher life satisfaction and positive emotions. |
| Study Findings | Shared meals are as predictive of happiness as income or employment status. |
| Trend in America | An increasing number of Americans are dining alone, with 1 in 4 reporting eating all their meals alone in 2023. |
| Implications of Research | The correlation between shared meals and happiness warrants further investigation into causal relationships. |
| Future Research Directions | Exploring whether individuals become happier as they share more meals. |
Summary
Shared meals and happiness are closely intertwined, as recent research indicates that sharing meals leads to a significant improvement in overall well-being. The findings suggest that regular dining with others can enhance life satisfaction and foster positive emotions, illustrating the vital role of social interactions in promoting mental health. Given the concerning trend of increasing solo dining experiences among Americans, encouraging communal meals may provide a straightforward yet effective avenue for enhancing social connections and individual happiness.

Treatable Genetic Disorders: A Breakthrough in Prenatal Care
Treatable genetic disorders represent an evolving field in prenatal care, shining a light on the remarkable advancements in medical science that allow early intervention for certain genetic conditions. Recent research has uncovered nearly 300 genetic disorders that can potentially be treated during pregnancy or shortly after birth, offering families hope and better outcomes. With the aid of genomic sequencing, healthcare providers can now identify these conditions earlier than ever, facilitating timely and effective fetal treatment options. This significant breakthrough in genetic conditions not only paves the way for proactive measures but also aims to reduce morbidity and mortality associated with untreated disorders. By integrating diagnostic information and fostering a collaborative approach among medical professionals, the focus on treatable genetic disorders empowers families with choices that could change their child’s life trajectory.
In the realm of maternal-fetal medicine, the focus on hereditary ailments that can be managed before birth is gaining traction. These manageable hereditary conditions are gaining widespread attention as researchers discover innovative solutions to provide early interventions. Understanding these actionable genetic findings allows practitioners to present expectant parents with vital information regarding emerging fetal therapies. As prenatal assessments become increasingly sophisticated, the emphasis on early detection and intervention in genetic anomalies is evident. The call for tailored prenatal strategies reinforces the significant shifts occurring in the approach to maternal health and fetal wellbeing.
Understanding Treatable Genetic Disorders
Treatable genetic disorders encompass a range of conditions identified and managed during pregnancy, offering promising avenues for intervention. In recent studies, nearly 300 such disorders were identified, highlighting the potential for prenatal care to significantly improve fetal health outcomes. This proactive approach allows for genomic sequencing to assess genetic conditions early on, empowering families with critical information that can lead to timely and effective treatments.
The essence of treating genetic disorders before birth lies in the advancements in prenatal diagnostics. With innovative techniques like genomic sequencing, healthcare professionals can pinpoint specific mutations linked to various disorders. By focusing on treatable genetic conditions, families can engage in informed decision-making about prenatal care and fetal treatment options, ultimately aiming to reduce the risks of morbidity and mortality associated with these conditions.
The Role of Prenatal Care in Genetic Disorder Management
Prenatal care plays a crucial role in managing genetic disorders by facilitating early detection and intervention strategies. Regular check-ups and advanced diagnostic testing, including ultrasound scans and genomic sequencing, allow healthcare providers to monitor potential fetal abnormalities. Early detection supported by prenatal care can lead to actionable insights, enabling timely interventions that improve health outcomes for both the fetus and the newborn.
Moreover, the introduction of a ‘treatable fetal findings list’, as proposed by researchers, enhances prenatal care by providing expectant parents with choices regarding their baby’s health management. This list comprises genetic conditions that are treatable or manageable shortly after birth, emphasizing the importance of early intervention. As families navigate their prenatal journey, access to such information can prove invaluable, guiding them in exploring appropriate treatment options.
Fetal Treatment Options for Genetic Conditions
Fetal treatment options have evolved significantly, thanks to advancements in medical technology and genetic research. For instance, conditions such as congenital heart defects or gastrointestinal disorders can often be treated with minimally invasive procedures while the fetus is still in utero. This proactive approach ensures that interventions occur before birth, allowing infants to start their lives with the best possible health outcomes.
In addition, several therapies may be initiated at birth, such as medication for specific genetic abnormalities or nutritional interventions for metabolic disorders. These treatments can drastically alter the course of genetic conditions, reducing the risk of long-term complications. By harnessing the potential of fetal medicine, healthcare providers can implement comprehensive treatment plans that not only address genetic conditions effectively but also enhance the quality of life for affected families.
The Importance of Early Intervention in Genetic Disorders
Early intervention remains a critical factor in managing genetic disorders effectively. The concept revolves around initiating treatment as soon as a disorder is diagnosed, which can lead to improved long-term outcomes. By providing timely access to therapies, many preventable complications can be avoided, ensuring healthier developmental trajectories for affected individuals.
Healthcare providers increasingly recognize the significance of integrating early intervention strategies into prenatal and postnatal care frameworks. This includes tailored approaches that consider each family’s unique circumstances, genetic background, and available treatment options. By fostering a collaborative relationship between families and caregivers, the health community can better navigate the complexities of genetic disorders and develop a supportive environment that maximizes health outcomes.
Genomic Sequencing: A Game-Changer in Prenatal Care
Genomic sequencing has revolutionized prenatal care, providing an unprecedented level of insight into fetal health. By analyzing the genetic material from the fetus, healthcare providers can identify abnormalities associated with multiple genetic disorders. This detailed understanding enables clinicians to diagnose conditions earlier in the pregnancy, ensuring timely interventions can be initiated.
The implications of genomic sequencing extend beyond diagnosis; they also encompass the potential for targeted therapies and tailored treatment plans. This technology enables families to better understand genetic predispositions and explore options that suit their unique needs. As genomic sequencing continues to evolve, it promises to enhance the landscape of prenatal care by providing data-driven pathways to safer, healthier pregnancies.
Ethical Considerations in Genetic Disorder Interventions
The integration of genetic findings into prenatal care raises several ethical considerations that must be thoughtfully addressed. As healthcare providers offer families a list of genetic disorders that can be treated during pregnancy, they must also navigate the implications of this information. Transparency is paramount, ensuring that parents fully comprehend both the possibilities and limitations associated with these treatments.
Furthermore, the emotional burden of receiving genetic information poses challenges for families. It is essential for healthcare teams to provide support and guidance, helping families to process the information while considering their options for prenatal care. Engaging genetic counselors and medical ethicists in this process can facilitate informed decision-making and ensure best practices are upheld in the care of expectant mothers and their babies.
Collaboration in Prenatal Care: A Multidisciplinary Approach
Effective management of genetic disorders during pregnancy requires a multidisciplinary approach, involving collaboration among various healthcare professionals. Geneticists, obstetricians, pediatricians, and nurses must work together to develop comprehensive care plans that guarantee access to vital resources and treatments. This teamwork fosters a holistic understanding of genetic conditions and facilitates timely interventions.
By collaborating across disciplines, healthcare providers can ensure that families receive clear and coherent information about available treatment options. This integrated approach not only enhances patient care but also empowers families to make informed decisions throughout their prenatal journey. By prioritizing collaboration, the healthcare community can effectively navigate the complexities of genetic disorders and optimize outcomes for both mothers and newborns.
Challenges in Addressing Genetic Disorders During Pregnancy
Despite significant advancements in prenatal care, challenges persist when addressing genetic disorders during pregnancy. One of the primary concerns includes the overwhelming amount of information that expectant parents may face, which can lead to anxiety and uncertainty. Offering a comprehensive yet digestible overview of treatable genetic disorders becomes imperative for healthcare providers.
Moreover, ethical dilemmas often arise regarding the extent to which families should be informed about potential genetic complications. Balancing honesty with compassion is key, as families may struggle with the implications of such knowledge. To mitigate these challenges, ongoing education and support from healthcare professionals are crucial, ensuring that families feel equipped to manage their prenatal and postnatal care effectively.
Future Directions in Prenatal Genetic Disorder Management
As research continues to evolve, the future of prenatal care for genetic disorders holds immense promise. Innovations in genomic technologies and therapeutic options are paving the way for enhanced detection and treatment strategies. The continuous exploration of new fetal therapies may lead to improved outcomes for genetic conditions that were previously deemed untreatable or manageable only postnatally.
Additionally, developing personalized medicine approaches based on individual genetic profiles will refine treatment plans for expectant families. By embracing the advancements in genomics and biotechnology, healthcare systems can foster a proactive mindset toward prenatal care, ultimately transforming the landscape of genetic disorder management and ensuring healthier generations ahead.
Frequently Asked Questions
What are treatable genetic disorders and how can genomic sequencing help in prenatal care?
Treatable genetic disorders refer to genetic conditions that can be effectively managed or treated, especially during pregnancy or shortly after birth. Genomic sequencing plays a crucial role in prenatal care by identifying these disorders early, allowing for timely interventions that can significantly improve health outcomes for the fetus.
What fetal treatment options are available for genetic conditions diagnosed during pregnancy?
Fetal treatment options for genetic conditions diagnosed during pregnancy may include medication management for congenital heart issues or procedural interventions for gastrointestinal disorders. Identifying treatable genetic disorders early can provide parents with choices that could alter the health trajectory of their child.
Why is early intervention important for treatable genetic disorders identified in prenatal care?
Early intervention is crucial for treatable genetic disorders because timely detection can reduce morbidity and mortality risks. By diagnosing conditions early in pregnancy or immediately after birth, families can access treatments that may prevent irreversible damage and improve the child’s quality of life.
How can parents learn about treatable genetic disorders during pregnancy?
Parents can learn about treatable genetic disorders during pregnancy through comprehensive prenatal care that includes discussions with obstetricians and genetic counselors. Genomic sequencing and prenatal screenings can help identify potential genetic issues, ensuring a proactive approach to fetal treatment options.
What challenges do families face when dealing with treatable genetic disorders found before birth?
Families may face challenges such as emotional distress from the diagnosis of treatable genetic disorders, overwhelming amounts of information, and ethical considerations regarding testing and treatment options. It is important for healthcare teams to provide support and clear communication to help navigate these complexities.
What is the goal of establishing a ‘treatable fetal findings list’ in prenatal care?
The goal of creating a ‘treatable fetal findings list’ in prenatal care is to empower families with information about genetic conditions that can be treated, enhancing the possibility for early interventions. This initiative aims to improve health outcomes while providing families with informed choices during pregnancy.
How are genetic disorders detected during prenatal care?
Genetic disorders are typically detected during prenatal care through advanced screenings such as non-invasive prenatal testing (NIPT), ultrasound examinations, and genomic sequencing. These methods help identify genetic conditions and determine appropriate fetal treatment options that can be initiated if necessary.
What role do healthcare professionals play in managing treatable genetic disorders during pregnancy?
Healthcare professionals, including geneticists and obstetricians, play a vital role in managing treatable genetic disorders during pregnancy by providing diagnoses, discussing treatment options, and supporting families through decision-making processes. Their collaboration ensures that patients receive comprehensive care tailored to their unique situations.
| Key Points | Details |
|---|---|
| New Study Findings | Identified nearly 300 genetic disorders that can be treated before birth or in the first week of life. |
| Actionable Conditions | Conditions can be treated with early intervention, potentially improving health outcomes. |
| Role of Genomic Sequencing | Vital for informing prenatal diagnoses, helping uncover treatable genetic disorders. |
| Development of Treatable Conditions List | A total of 296 genetic conditions identified for early intervention opportunities. |
| Ethical Considerations | Overwhelming amount of information may complicate patient understanding and decision-making. |
| Collaboration Importance | Emphasizes teamwork among clinicians, genetic counselors, and ethicists for comprehensive patient care. |
Summary
Treatable genetic disorders represent a significant advancement in prenatal care, offering new opportunities for intervention before birth. With a recent study identifying nearly 300 such conditions, medical professionals are now empowered to detect potential genetic disorders early, leading to timely treatments that can greatly improve outcomes for affected infants. This proactive approach is crucial in addressing the morbidity associated with undiagnosed genetic issues and ensuring that families have access to the necessary information and support throughout the process.
Manage Stress During an Apocalypse: Strategies for Survival
Managing stress during an apocalypse requires a multifaceted approach that focuses on psychological resilience and community solidarity. As we face the potential chaos of climate crises, pandemics, and societal upheaval, understanding effective stress management techniques becomes essential for survival. Expert insight from psychology professor Athena Aktipis reveals that embracing adventure, gathering diverse information, and fostering community support are vital coping strategies. By leveraging these strategies, individuals can better navigate the uncertainties of apocalyptic scenarios and emerge with a sense of agency and readiness. In a world where ambiguity reigns, mastering the art of stress management is not just beneficial; it’s a crucial skill for enduring and thriving in tumultuous times.
In challenging times, particularly during catastrophic events, the importance of effective coping mechanisms and communal assistance cannot be overstated. Surviving dire scenarios demands a reevaluation of our mental health strategies and social ties, as we learn to adaptively handle mounting pressures. The recent discourse around stress management suggests that understanding the dynamics of both individual and collective wellbeing is crucial. By applying frameworks focused on risk awareness and interpersonal support, we can better prepare ourselves for unforeseen challenges. Thus, the shift towards community-driven resilience is not merely a novel concept but an essential part of navigating life’s unpredictable nature.
Understanding Stress Management in Apocalyptic Times
In the face of global crises such as climate change, pandemics, and social upheaval, effective stress management becomes crucial. The tumultuous nature of current events can leave individuals feeling overwhelmed, but there are strategies to navigate these challenges. Stress management during an apocalypse, as detailed by psychologist Athena Aktipis, involves a multifaceted approach that includes gathering accurate information, reassessing the sources of stress, and embracing community support. By reevaluating how we perceive risks and approaching them from different perspectives, we can significantly reduce anxiety and improve our mental resiliency.
Moreover, engaging with a community can bolster our coping strategies. In uncertain times, having a support network provides emotional and practical benefits, creating an environment where mutual aid can flourish. Learning from shared experiences and collaborating on ways to tackle challenges can empower individuals, making stressors seem more manageable. Building these connections not only aids in surviving apocalyptic scenarios but also fosters a sense of belonging and collective purpose, which is vital for mental health.
Coping Strategies for Surviving an Apocalypse
To thrive amidst chaos, developing coping strategies is essential. Athena Aktipis emphasizes the importance of looking at potential threats from various angles, suggesting that a well-rounded understanding can inform our actions and alleviate unnecessary stress. For instance, instead of fixating on a singular risk, by gathering diverse insights from different sources, we can better assess our situation and prioritize our responses. This might involve reaching out to individuals with expertise different from our own, enriching our knowledge base, and identifying effective action plans that cater to our immediate needs.
Implementing practical coping mechanisms is equally important. Elements such as routine, mindfulness, and engaging in hobbies can buffer the effects of stress during tumultuous times. For Aktipis, the acronym CHESS — which stands for Curiosity, Humor, Entertaining, Storytelling, and Socializing — offers a playful yet profound framework to manage stress. By integrating these activities into our lives, we not only enhance our wellbeing but also cultivate connections that can serve us during harder times. These shared moments provide sustenance that prepares us to face the unpredictability of an apocalypse.
The Role of Community Support in Stress Management
Community support plays a critical role in managing stress, particularly during crises. According to Aktipis, cooperation and mutual aid can transform an individual’s experience of an apocalypse into something more survivable. The relationships we build, whether with family, friends, or neighbors, can serve as buffers against stress. Through collaborative efforts, individuals can share resources, offer emotional backing, and enhance collective resilience, ultimately reducing the weight of individual burdens that come with managing stress in uncertain times.
Moreover, the concept of social insurance, as demonstrated through the Maasai people’s Osotua system, illustrates how community bonds can support individuals during difficult moments. By fostering an environment of mutual assistance, where people help one another without expectation of immediate return, we can create a safety net that offers psychological relief and promotes a sense of belonging. This foundational support can empower individuals, enabling them to face adversities with greater confidence and mental fortitude.
From Panic to Preparedness: Changing Our Mindset
A significant aspect of surviving apocalyptic scenarios involves the transformation of our mindset from panic to preparedness. Aktipis suggests that rather than succumbing to despair, we should view crises as opportunities for learning and growth. This shift allows us to reframe our thinking, emphasizing the potential for resilience and adaptation in uncertain environments. By embracing a proactive approach, we can develop strategies that not only help manage stress but also equip us to handle future challenges more effectively.
This perspective encourages individuals to engage in activities that stimulate curiosity and creativity, rekindling the desire to explore and experiment. By fostering a mindset focused on discovery, individuals can mitigate feelings of helplessness associated with an apocalypse. Instead of viewing the future with dread, we can cultivate hope through preparation and adaptability, ultimately allowing us to thrive rather than merely survive in the face of adversity.
Applying Game Theory to Collective Survival Strategies
Athena Aktipis emphasizes the relevance of game theory in developing collective strategies for survival during apocalyptic times. By understanding that success does not have to be a zero-sum game, we can change the narrative from competition to cooperation. This approach encourages collaboration among individuals and communities, leading to the creation of shared resources that can sustain us in times of need. By working together to expand the ‘pie’ of available resources, we ensure that everyone benefits, rather than feeling compelled to fight for limited resources.
The application of game theory can unlock new pathways for cooperation and mutual support. For instance, community-driven projects that focus on pooled resources or shared knowledge not only alleviate individual stress but also strengthen the bonds between community members. Recognizing that we are all navigating the same uncertain terrain can inspire a collective response, fostering a spirit of unity even in the most challenging scenarios. In this way, cooperation becomes not just a moral imperative but a strategic necessity.
Exploring Emotional Wellness in Crisis Scenarios
In the context of crisis management, exploring emotional wellness is vital for maintaining mental health. Aktipis highlights the importance of identifying one’s emotional needs and addressing them proactively. This might involve engaging in practices that promote emotional healing, such as journaling, meditation, or sharing experiences with trusted individuals. By acknowledging our feelings and the stressors associated with them, we can better prepare ourselves to face the complexities of apocalyptic situations.
Furthermore, emotional wellness is interconnected with physical health. Engaging in regular physical activity, maintaining a balanced diet, and ensuring adequate rest can significantly enhance our emotional resilience. The importance of nurturing both our mind and body cannot be overstated during stressful times. By fostering emotional wellness, we build a stronger foundation for coping with the adversities that come with surviving apocalyptic challenges, ensuring that we are not only surviving but thriving, even when confronted with dire circumstances.
Harnessing the Power of Humor During Hard Times
Humor serves as a powerful coping mechanism in times of crisis, offering a respite from stress and providing perspective. Aktipis encourages incorporating humor as a fundamental part of stress management strategies. By finding amusement in our circumstances, we can alleviate tension and foster a lighter atmosphere within ourselves and in our communities. This is particularly beneficial during apocalyptic situations when fear and anxiety may dominate our thoughts.
In addition, humor can be a means of creating connections among individuals. Shared laughter can strengthen community bonds, fostering an environment of support and understanding. Aktipis’ emphasis on storytelling and entertainment reflects the idea that humor not only promotes emotional wellness but also enhances our collective ability to withstand challenges. By prioritizing joy and laughter, we cultivate resilience that can help us navigate the complexities of living in a world filled with uncertainty.
Preparing for the Unexpected: Lifelong Learning and Adaptability
One of the pillars of surviving apocalyptic scenarios lies in the commitment to lifelong learning and adaptability. Embracing new knowledge and skills enhances our ability to navigate complexities effectively. Aktipis argues that understanding the diverse risks we may face allows us to prepare better, not only for immediate threats but also for unforeseen future challenges. This proactive stance can reduce stress levels by instilling a sense of readiness and competence.
Additionally, adaptability is crucial in managing stress during an apocalypse. The ability to pivot and adjust our strategies based on emerging information can make all the difference in stressful situations. This aligns closely with Athena Aktipis’ framework, emphasizing the need to gather information thoughtfully and make informed decisions. By fostering a culture of continuous improvement and adaptability, individuals and communities can enhance their resilience and succeed in the face of adversity.
Creating Meaning from Crisis: A New Perspective on Apocalyptic Events
Instead of viewing apocalyptic events solely as catastrophes, Aktipis urges us to consider them as opportunities for personal and societal growth. Understanding crises as pivotal moments can offer new insights into our values, priorities, and connections with others. By reframing our perspective on these events, we can cultivate a deeper sense of purpose and meaning that transcends fear and anxiety.
This approach is restorative, empowering individuals to forge new paths forward when faced with challenges. Embracing the lessons learned during these times can lead to profound changes in how we relate to ourselves and each other, ultimately guiding us toward more holistic forms of stress management. By finding meaning in adversity, we cultivate resilience that can sustain us well beyond any immediate challenges.
Frequently Asked Questions
How can I manage stress during an apocalypse effectively?
Managing stress during an apocalypse involves utilizing effective stress management techniques that encourage community support and open communication. Stay informed about potential threats, engage in activities that foster curiosity, humor, and storytelling, and maintain connections with others to cultivate a supportive network. These coping strategies can help mitigate feelings of anxiety and improve overall resilience.
What are some coping strategies for dealing with stress during apocalyptic scenarios?
Coping strategies for managing stress during apocalyptic scenarios include gathering information from credible sources, assessing risks from multiple perspectives, and utilizing community support. Practices such as mindfulness, engaging in physical activity, and fostering social connections can also be effective in relieving stress in these uncertain times.
How important is community support in managing stress during an apocalypse?
Community support is crucial for managing stress during an apocalypse. Building strong relationships and mutual aid networks can provide emotional and practical assistance, making it easier to cope with challenges. Engaging with others enhances feelings of safety and reduces feelings of isolation, contributing significantly to effective stress management.
What role does understanding risk play in managing stress during an apocalypse?
Understanding risk is vital in managing stress during an apocalypse. By gathering information and analyzing threats clearly, individuals can make informed decisions about their safety and priorities. This knowledge helps to reduce anxiety by distinguishing between actual dangers and perceived threats, allowing for more focused coping strategies.
What is the importance of adaptability in surviving apocalyptic scenarios and managing stress?
Adaptability is essential for surviving apocalyptic scenarios and managing stress effectively. Being flexible in your approach to challenges allows you to respond to changing circumstances and threats. Embracing new information and remaining open to different solutions can alleviate stress and enhance resilience as you navigate uncertain times.
How can Athena Aktipis’ insights help with stress management during an apocalypse?
Athena Aktipis’ insights highlight the importance of community, curiosity, and proactive information gathering in managing stress during an apocalypse. Her framework encourages individuals to assess threats from multiple angles and engage with diverse perspectives, which can foster better decision-making and reduce panic, thereby improving overall resilience in stressful situations.
What activities can contribute to stress relief during an apocalyptic situation?
Activities that contribute to stress relief during an apocalyptic situation include engaging in hobbies that spark curiosity, practicing humor, storytelling, and maintaining social interactions. Additionally, physical exercise and creative outlets can also serve as effective coping mechanisms, allowing individuals to manage their stress and maintain a sense of normalcy.
How does a mindset shift help with stress management during an apocalypse?
A mindset shift helps with stress management during an apocalypse by allowing individuals to view challenges as opportunities for growth rather than purely as threats. Fostering a perspective that encourages curiosity and playfulness can enhance resilience, reduce anxiety, and provide motivation to engage in positive coping strategies.
| Key Points |
|---|
| Understand that crises are part of human existence and gather information to manage stress. |
| Embrace cooperation and community as vital tools for survival. |
| Recognize the ambiguity in threat identification; assess risks thoughtfully. |
| Change your mindset to build resilience through ‘apocalyptic sustenance’ which includes fun and curiosity. |
| Utilize social activities to forge connections for mutual aid during emergencies. |
| Emphasize that survival does not have to be a zero-sum game; collaboration creates better outcomes. |
| Learn from traditional systems of support like the Maasai Osotua to manage risk through social bonds. |
Summary
To manage stress during an apocalypse, understanding the importance of gathering information and embracing community support is essential. As highlighted by psychology professor Athena Aktipis, crises present both challenges and opportunities for resilience. Engaging with diverse perspectives, fostering relationships, and reorienting our priorities can significantly ease our stress levels. By adopting a mindset that sees crises not merely as disasters but as opportunities for growth and collaboration, we can thrive even in uncertain times.
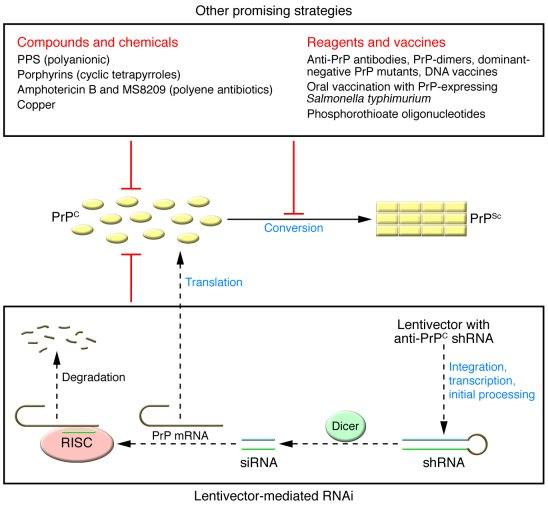
Prion Disease Treatment: A Breakthrough in Gene Editing
Prion disease treatment has made significant strides recently thanks to pioneering research led by dedicated scientists at the Broad Institute of MIT and Harvard. These rare and devastating disorders, including Creutzfeldt-Jakob disease and fatal familial insomnia, are caused by misfolded proteins that wreak havoc in the brain. A groundbreaking study has introduced a novel gene-editing therapy, which holds promise for potentially reducing prion protein levels, thereby extending the lifespan of affected individuals significantly in laboratory settings. Researchers, motivated by their personal connections, are optimistic that further advancements will pave the way for human clinical trials. With the collaborative effort of experts in HMS neurology research, the future of prion disease treatment appears more hopeful than ever before.
The exploration of therapies for prion diseases has opened avenues for innovative medical treatments targeting these life-threatening neurological conditions. Characterized by the accumulation of malformed proteins, prion disorders unveil a complex challenge for researchers aiming to reverse their effects. Approaches involving advanced genetic modification techniques, such as gene editing, are being actively developed to counteract the detrimental impact of misfolded prion proteins. As the scientific community rallies around findings related to these conditions, including inherited forms and those resulting from sporadic occurrences, the potential for effective interventions grows. The commitment of patient-researchers to this cause illuminates the human element driving these transformative studies.
Innovative Approaches to Prion Disease Treatment
Researchers are now leveraging breakthrough technologies such as gene editing therapy to address prion diseases, which are known for their devastating consequences. These disorders, including notable conditions like Creutzfeldt-Jakob disease and fatal familial insomnia, have long eluded effective treatments. Recent advancements in the lab, particularly by teams at Harvard’s Broad Institute, have sparked hope. Their promising findings indicated that a precise alteration in the prion protein gene could lead to a significant reduction in misfolded proteins associated with prion diseases, highlighting a potential pathway for treatment.
The innovative methods are based on a technique called single-base editing—an approach that allows researchers to target and modify specific genes effectively. By employing a novel adeno-associated virus as a delivery system, the research team successfully integrated this technique into their therapeutic framework. This advancement could significantly reduce prion protein levels in human cells, paving the way for future human trials and marking a pivotal moment in prion disease treatment.
The Personal Drive Behind Prion Disease Research
The journey of developing treatments for prion disease is deeply personal for researchers like Sonia Vallabh and Eric Minikel, who not only work in the field but are also affected by it. Vallabh’s firsthand experience with fatal familial insomnia, coupled with the loss of her mother to the same condition, fuels her commitment to finding a cure. This personal connection highlights the importance of patient-scientists who bring unique perspectives to medical research, often transforming their grief into a motivational force that drives scientific inquiry.
Their story exemplifies how personal stakes can shape research trajectories. Vallabh and Minikel transitioned from their respective backgrounds in law and computer science to immerse themselves in the complexities of prion diseases, showcasing a merger of personal passion and scientific ambition. Their collaboration with established researchers, including David Liu, demonstrates how diverse expertise can accelerate progress toward effective therapies. Their narrative emphasizes that behind each scientific challenge are individuals whose lives are impacted, advocating for advancements in treatment options.
Understanding the Mechanism of Prion Diseases
Prion diseases are a category of neurodegenerative conditions caused by abnormal misfolding of prion proteins in the brain, leading to severe neurological impairment. Conditions like Gerstmann-Sträussler-Scheinker disease and Creutzfeldt-Jakob disease exemplify the spectrum of prion-related disorders, which often result in dementia and eventually death. Researchers are working diligently to disentangle the complex mechanisms that govern these protein misfolding events, thus developing innovative strategies for intervention.
One of the critical areas of focus is the genetic basis of these conditions, as approximately 15 percent of prion disease cases are attributed to inherited mutations within the prion protein gene. By understanding how these mutations influence protein behavior and the resultant pathology, researchers can seek tailored treatments aimed at correcting or compensating for these defects. This intricate understanding underpins the development of gene editing therapy, offering crucial insights into the future of prion disease treatment.
Collaborative Research: The Key to Progress
The fight against prion diseases underscores the importance of collaboration among scientists, clinicians, and patient advocates. The joint efforts between Vallabh and Minikel, along with their research partners, highlight a collective ambition to push the boundaries of existing science. By pooling their expertise and resources, they not only advance the field but also foster a supportive environment that enhances creativity and innovation in tackling these complex disease mechanisms.
Collaborative research offers multiple benefits: it accelerates the pace of discovery, optimizes the use of diverse technologies, and enriches the research environment with varied perspectives. The ongoing dialogue among different labs, such as those at the Broad Institute and HMS, exemplifies how interdisciplinary partnerships can effectively address the nuances of prion disease research. This synergy of knowledge and shared goals plays a pivotal role in uncovering viable treatment pathways for patients afflicted by these devastating conditions.
Challenges in Human Trials for Prion Disease Therapy
Despite the promising advancements in laboratory research, moving towards human trials for prion disease therapies presents a myriad of challenges. The unique properties of prion proteins, notorious for their infectious nature, necessitate rigorous consideration of safety protocols and regulations. Past incidents have underscored the risks involved in studying human prion proteins, forcing researchers to adopt cautious approaches in their investigations.
As the team progresses towards clinical applications, they must refine their gene editing techniques to ensure both efficacy and safety. This involves enhancing the precision of delivery systems like adeno-associated viruses to minimize unintended consequences on non-target cells. Rigorous testing, evaluation, and regulation are essential to pave the way for successful human trials, ultimately contributing to sustainable treatment options for patients impacted by prion diseases.
Funding: A Crucial Element in Prion Research
Financial investment plays a critical role in advancing prion disease research and the development of therapeutic options. Funding sources, such as the National Institutes of Health and private foundations like the Prion Alliance, provide essential resources necessary to support innovative studies. These financial contributions help cover the costs of experimental materials, labor, and necessary technology, facilitating groundbreaking discoveries in the field.
Moreover, proper funding allows researchers to pursue ambitious projects that may otherwise seem unattainable. It fosters an environment where curious minds can explore the complexities of diseases and collaborate to yield innovative solutions. As demonstrated by the work of Vallabh, Minikel, and their collaborators, dedicated funding mechanisms empower scientific inquiry that could potentially lead to life-saving therapies for individuals living with prion diseases.
The Future of Prion Disease Treatment: What Lies Ahead
The future of prion disease treatment appears increasingly optimistic as researchers continue to explore innovative strategies and technologies. The recent advancements in gene editing therapy exemplify the potential for transformative treatments that could change the lives of those afflicted by these devastating disorders. As research evolves, it is crucial to maintain momentum through interdisciplinary collaborations and sufficient funding.
Looking ahead, a concerted effort to refine gene editing techniques, coupled with ongoing studies in animal models, could hasten the timeline for clinical applications. The ultimate goal is to translate these laboratory findings into effective therapies for patients suffering from conditions like Creutzfeldt-Jakob disease and fatal familial insomnia. As the field progresses, the importance of remaining vigilant in addressing ethical challenges and trial regulatory processes will shape the future landscape of prion disease treatment.
Rare but Deadly: The Impact of Prion Diseases
Prion diseases are among the most chilling and rare forms of neurodegenerative disorders. Their rarity, however, does not diminish their severity or the devastating impact they can have on individuals and families. As these diseases progress, victims typically experience cognitive decline, loss of motor control, and eventually death. The psychological strain on families dealing with such a diagnosis is immense, underscoring the need for effective research and treatment options.
In the broader context of public health, understanding prion diseases contributes to awareness and education around neurodegenerative disorders as a whole. As excitement builds around potential treatments developed through innovative research approaches, it is essential to promote knowledge about these conditions. This facilitating public discourse can help garner support for ongoing studies and prepare communities for the challenges surrounding prion diseases.
Gene Editing Therapy: A Beacon of Hope
Among the innovative strategies being explored for the treatment of prion diseases, gene editing therapy stands out as a beacon of hope. Research efforts aimed at altering the prion protein gene have shown remarkable promise, revealing potential pathways for significantly reducing or even halting the progression of these often-fatal conditions. The ability to accurately edit genes may enable the development of lifelong interventions that could change the trajectory of prion diseases entirely.
By focusing on the very roots of the problem—misfolded proteins—gene editing therapy introduces a new paradigm in treating neurodegenerative disorders. Although the road to implementation is fraught with challenges, the achievements thus far inspire optimism among both researchers and patient advocates. As the field evolves, ongoing integration of cutting-edge technologies will likely yield successful therapeutic outcomes.
Frequently Asked Questions
What recent advancements have been made in prion disease treatment through gene editing therapy?
Recent research published in *Nature Medicine* highlights a promising gene editing therapy that shows potential in treating prion diseases such as Creutzfeldt-Jakob disease and fatal familial insomnia. This therapy involves altering a single base in the prion protein gene, resulting in a 50% reduction of harmful protein levels in laboratory mice, which subsequently extended their lifespans by 52%.
How does gene editing therapy target prion diseases like Creutzfeldt-Jakob disease?
Gene editing therapy aims to mitigate prion diseases such as Creutzfeldt-Jakob disease by modifying the prion protein gene responsible for producing misfolded proteins. Researchers have developed a technique that employs a base editor inserted into a viral vector, allowing for targeted alterations in DNA that reduce toxic protein levels, which is crucial for effective prion disease treatment.
What role do patient-scientists play in the research and treatment of prion diseases?
Patient-scientists, like Sonia Vallabh and Eric Minikel, are integral to advancing prion disease treatment. Their personal connection to fatal familial insomnia propels their research efforts, focusing on developing gene editing therapies. Their firsthand experience enhances motivation and aids in steering research towards effective solutions for prion diseases.
What challenges remain before gene editing therapies can be applied to human prion disease treatment?
Despite promising advancements in gene editing therapies for prion diseases, significant challenges lie ahead. The pathway to human trials involves meticulous refinement of the base editor for safer and more efficient delivery, minimizing risks associated with potential prion protein exposure, and ensuring targeted integration to avoid non-target tissue effects.
Why is it significant that prion disease treatment research utilizes mouse models?
Utilizing mouse models in prion disease treatment research is significant because it increases the likelihood that findings will translate effectively to human applications. These models closely mimic the human form of prion diseases, allowing researchers to study the efficacy of gene editing therapies in reducing protein levels and extending lifespan, which are crucial indicators for future human trials.
| Key Points | Details |
|---|---|
| Promising Research | A new gene-editing therapy offers hope for prion disease treatment. |
| Significant Findings | Altering a single gene base in mice reduced harmful protein levels by 50%, extending lifespan by 52%. |
| Patient-Scientist Collaboration | Sonia Vallabh, a prion disease patient, and Eric Minikel lead their own lab focusing on prion disease research. |
| Ongoing Challenges | Numerous milestones must be navigated before human trials can begin. |
| Collaborative Efforts | Research involves interdisciplinary teams and support from institutions and funding sources. |
| Caution Needed | The infectious nature of prion diseases complicates future research and human trials. |
Summary
Prion disease treatment has garnered significant attention due to a recent breakthrough in gene-editing technology. Researchers have demonstrated that by altering a single base in the gene responsible for producing harmful prion proteins, they can reduce protein levels significantly in laboratory mice, providing hope for future therapies. While the journey to human trials is fraught with challenges, the collaboration between patient-scientists and dedicated researchers signals a promising pathway toward innovative treatments for this devastating group of diseases.