
AI Tool Pediatric Cancer Prediction Unveiled by Harvard Study
The AI tool pediatric cancer prediction is revolutionizing the way specialists predict cancer recurrence in young patients. A groundbreaking study from Mass General Brigham has shown that this sophisticated AI model can analyze multiple MRI scans over time to assess the risk of pediatric cancer relapse, significantly outpacing traditional prediction methods. This advancement is particularly crucial for children diagnosed with gliomas, as understanding the risk of glioma recurrence can lead to more effective and less stressful follow-up care. By harnessing the power of temporal learning in AI, researchers are able to identify early warning signs of potential relapse, paving the way for improved patient outcomes. As AI in medicine continues to evolve, tools like these promise to transform how healthcare teams navigate complex conditions such as pediatric cancer.
The utilization of advanced artificial intelligence techniques for predicting pediatric cancer probabilities is gaining momentum within the healthcare sector. This innovative approach leverages machine learning algorithms to evaluate patterns in medical imaging data, offering valuable insights into the likelihood of pediatric tumor recurrence. By employing comprehensive MRI scan analyses, health professionals can better strategize follow-up care and treatments tailored to individual needs, especially in cases involving gliomas. As the field of AI in healthcare matures, the integration of temporal learning models presents exciting possibilities for enhancing predictive accuracy and patient management. Overall, the quest for effective tools to detect and combat pediatric cancer remains a pivotal focus for researchers and healthcare providers alike.
Understanding Pediatric Cancer Recurrence Through AI
Pediatric cancer recurrence, particularly in cases of gliomas, represents a significant challenge for healthcare providers and families alike. The introduction of AI tools specifically designed to predict relapse risk has transformed how these cases are managed. By analyzing longitudinal MRI scans, these tools leverage sophisticated algorithms to identify patterns that may not be visible in isolated images. This not only helps in early detection but allows healthcare teams to tailor their follow-up strategies according to individual risk profiles.
The ability to accurately assess recurrence risk can greatly relieve the anxiety for families and reduce the number of unnecessary imaging procedures. AI can identify patients who have a lower risk and allow them to have less frequent follow-ups, making post-treatment life more manageable for these children. In contrast, high-risk patients can receive timely interventions, improving their chances of avoiding relapse and ultimately leading to better outcomes in pediatric oncology.
Frequently Asked Questions
How does the AI tool for pediatric cancer prediction improve the accuracy of detecting cancer relapse?
The AI tool for pediatric cancer prediction leverages temporal learning to analyze multiple MRI scans over time, enhancing its ability to identify subtle changes linked to pediatric cancer relapse. This approach allows the tool to predict glioma recurrence with an accuracy of 75-89%, significantly outpacing traditional methods which rely on single scans.
What role does temporal learning play in AI for pediatric cancer prediction?
Temporal learning is crucial for AI in pediatric cancer prediction as it enables the model to assess changes in MRI scans taken at different times post-surgery. By synthesizing data from several scans, the AI can more accurately predict the risk of glioma recurrence and improve patient outcomes.
Why is MRI scan analysis important in predicting pediatric cancer relapse?
MRI scan analysis is vital in predicting pediatric cancer relapse as it provides detailed imaging that helps detect glioma recurrence. The AI tool enhances this analysis by using temporal learning, allowing for a more comprehensive understanding of tumor behavior over time.
What is glioma recurrence and how does AI help predict it in pediatric patients?
Glioma recurrence refers to the return of brain tumors in pediatric patients after treatment. The AI tool specifically designed for pediatric cancer prediction uses advanced algorithms to analyze multiple MRI scans, improving the prediction of recurrence and enabling timely interventions.
In what ways can AI in medicine transform care for pediatric cancer patients?
AI in medicine has the potential to transform care for pediatric cancer patients by providing more accurate predictions of relapse, minimizing unnecessary imaging, and guiding timely treatments. With tools for pediatric cancer prediction, healthcare providers can tailor follow-up care based on individual risk assessments.
How can the findings from the Mass General Brigham study on pediatric cancer prediction impact clinical practices?
The findings from the Mass General Brigham study on pediatric cancer prediction could lead to significant changes in clinical practices by enabling the development of personalized follow-up strategies. This may include reducing scanning frequency for low-risk patients and initiating targeted therapies for those identified as high-risk.
What are the potential future applications of the AI tool for pediatric cancer prediction?
The potential future applications of the AI tool for pediatric cancer prediction include broader use in various types of cancers requiring longitudinal imaging, allowing healthcare professionals to optimize monitoring strategies and interventions based on AI-driven insights.
What challenges remain before the AI tool for pediatric cancer prediction can be used clinically?
Before clinical application, the AI tool for pediatric cancer prediction must undergo further validation in diverse settings and clinical trials to ensure its effectiveness and reliability for guiding treatment decisions in pediatric cancer care.
| Key Point | Details |
|---|---|
| AI Tool Advantage | The AI tool predicts relapse risk in pediatric cancer patients with greater accuracy than traditional methods. |
| Temporal Learning Technique | This innovative technique enables the AI to assess multiple brain scans taken over time, enhancing prediction accuracy. |
| Research Collaboration | Involves collaboration among Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. |
| Study Results | The AI predicted recurrence of gliomas with 75-89% accuracy, compared to 50% using single scans. |
| Clinical Implications | Potential to reduce unnecessary imaging for low-risk patients and improve treatment for high-risk patients. |
Summary
The AI tool pediatric cancer prediction has been shown to significantly enhance the ability to predict cancer recurrence in pediatric patients, especially those with brain tumors like gliomas. By utilizing advanced techniques such as temporal learning, this AI model analyzes multiple scans over time, thereby improving accuracy and potentially transforming how clinicians approach follow-ups and treatment. As research progresses, further validation and clinical trials will be crucial in determining the practical applications of this technology in pediatric oncology.

Pediatric Cancer Relapse Prediction: AI Outperforms Traditional Methods
Pediatric cancer relapse prediction is revolutionizing how medical professionals assess the risk of recurrence in young patients, particularly those suffering from brain tumors like gliomas. A recent study by researchers at Mass General Brigham highlights the capabilities of an advanced AI tool that analyzes multiple MRI images over time, offering insights that far surpass traditional methods. With an impressive predictive accuracy of 75-89% for low- or high-grade gliomas, this technology not only promises to enhance patient care but also alleviates the anxiety felt by families subjected to constant follow-up imaging. The implementation of temporal learning in medicine allows the AI to recognize subtle changes across several scans, thus refining the prediction process for pediatric oncology. As this AI in pediatric cancer continues to evolve, it holds the potential for significant advancements in identifying patients at high risk for brain tumor recurrence, ultimately leading to more tailored treatment approaches.
The analysis of pediatric cancer recurrence risk is critical in delivering effective medical care for children battling serious illnesses. Emerging techniques in artificial intelligence provide fresh avenues for predicting relapse risk, particularly in the context of brain tumor management. By leveraging sequential MRI imaging in pediatric oncology, researchers can gain deeper insights into tumor behavior over time, moving beyond the limitations of traditional single-scan assessments. This innovative approach fosters a greater understanding of glioma recurrence, enhancing our capabilities to respond when dealing with the challenges of childhood cancers. As we explore these developments in predictive analytics, it becomes increasingly evident that integrating advanced technologies into medical practice can optimize patient outcomes and refine therapeutic strategies.
The Evolution of AI in Pediatric Oncology
Artificial Intelligence (AI) has made significant strides in various fields, and its application in pediatric oncology is proving to be revolutionary. By utilizing advanced algorithms and machine learning techniques, researchers are developing tools that can analyze vast amounts of medical data, including MRIs and other imaging studies. AI’s capacity to process complex datasets quickly and accurately offers a new frontier in predicting outcomes for children diagnosed with various forms of cancer, particularly brain tumors such as gliomas.
As these AI models evolve, they increasingly incorporate diverse methodologies including temporal learning, which enhances the predictive capabilities for cancer recurrence. The integration of AI in medicine not only streamlines patient assessments but also helps in crafting personalized treatment plans, thus potentially reducing the physical and emotional burden faced by young patients and their families.
Pediatric Cancer Relapse Prediction: A Game Changer
Predicting the relapse risk in pediatric cancer patients is a critical aspect of their care. Traditional methods have often relied on limited data points, but AI tools, with their ability to analyze serial imaging data, are changing the landscape of cancer recurrence prediction. One recent study highlighted that AI can predict the risk of relapse with accuracy rates between 75% and 89% — a significant improvement over traditional predictive methods which only achieved about 50% accuracy. This advancement underscores the potential of AI in better identifying which patients may require intensified monitoring or modified treatment strategies post-surgery.
Moreover, by accurately predicting the likelihood of recurrence, healthcare providers can tailor follow-up protocols more effectively. For instance, patients identified as low-risk based on AI analysis may experience reduced frequency of MRIs, thereby alleviating some of the associated stress and discomfort for both the patients and their families. This personalized approach could lead to improved quality of life during the post-treatment phase, highlighting the transformative potential of AI in pediatric cancer care.
MRI Imaging Technology and Its Role in Pediatric Oncology
Magnetic Resonance Imaging (MRI) plays a crucial role in pediatric oncology, especially for diagnosing and monitoring tumors. In the context of brain tumors such as gliomas, MRI is indispensable for understanding tumor size, location, and progression. Traditionally, physicians have relied on static images from single scans to make critical treatment decisions; however, this method has its limitations in accurately assessing the dynamic nature of tumors.
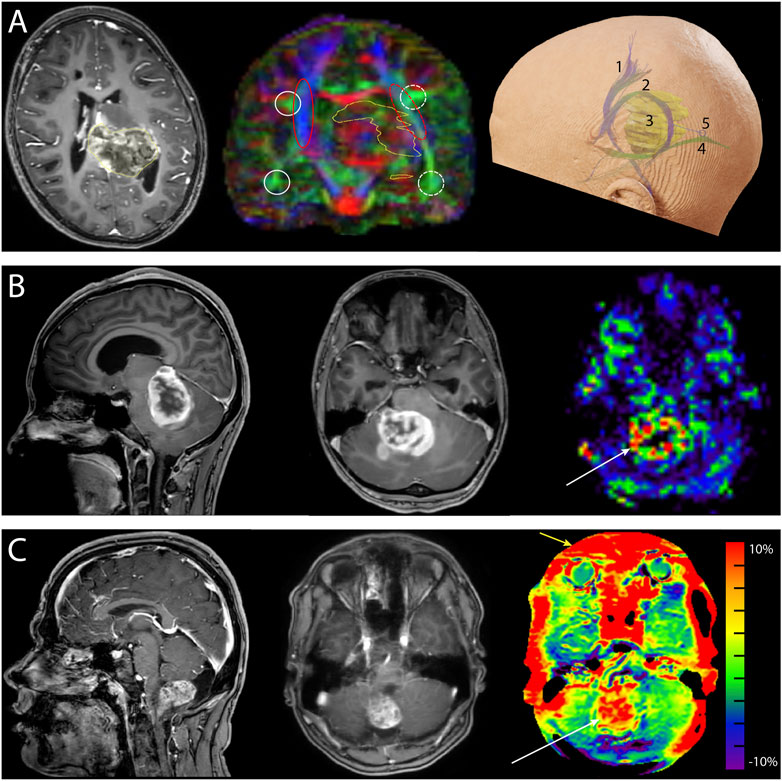
The advent of AI and temporal learning technologies is set to enhance the capabilities of MRI in pediatric oncology. By analyzing a series of scans over time, AI can detect subtle changes in the tumor’s behavior that may not be visible in a single snapshot. This approach provides a more comprehensive understanding of tumor dynamics, ultimately aiding in the prediction of recurrence and guiding timely therapeutic interventions.
Exploring Temporal Learning in Medicine
Temporal learning is an innovative approach within the realm of artificial intelligence that focuses on analyzing data across time rather than in isolated snapshots. In pediatric oncology, particularly when monitoring gliomas, utilizing historical imaging data offers deeper insights into tumor behavior and treatment response. The ability to sequence a patient’s MRIs chronologically allows AI systems to learn from patterns over time, enhancing the predictive accuracy regarding cancer recurrence.
This methodology represents a significant advancement over traditional predictive models, which typically do not consider the temporal aspect of medical data. As research continues to support the efficacy of temporal learning, it opens up new avenues for improving patient outcomes in pediatric cancer. The long-term goal is to integrate these innovative techniques into clinical settings, offering tools that not only enhance prediction models but also improve the overall therapeutic strategies for young patients.
The Promise of AI in Predicting Brain Tumor Recurrence
The ability to predict brain tumor recurrence in pediatric patients accurately is a paramount challenge in oncology. Researchers are increasingly turning to artificial intelligence to tackle this issue, employing AI tools that analyze multiple MR images taken over time to identify changes that may signal a risk of relapse. The integration of AI-driven predictions has shown success by substantially improving accuracy, allowing clinicians to make better-informed decisions regarding patient management.
The success of AI in predicting brain tumor recurrence can significantly alter the landscape of pediatric oncology. With tools that provide earlier insights into a potential relapse, healthcare providers can implement preventive strategies or adjust treatment protocols promptly. This proactive approach stands to improve outcomes and could potentially save lives, marking a pivotal shift towards personalized and data-driven care in pediatric cancer treatment.
Transforming Pediatric Cancer Care Through Data Analysis
Data analysis is at the heart of enhancing pediatric cancer care, particularly in the realm of predicting outcomes and tailoring treatment strategies. The integration of AI tools helps researchers and clinicians sift through extensive datasets derived from diverse sources such as MRI scans, clinical histories, and treatment outcomes. This analysis not only helps in predicting relapse but also in understanding the broader implications of treatment decisions across different demographics and tumor types.
Furthermore, the continuous collection and analysis of patient data through these advanced AI systems can lead to more personalized medicine approaches. As more pediatric patients are monitored and data is accumulated, the insights gained will refine risk assessments and provide invaluable information that can shape future clinical guidelines and treatment protocols effectively. In this way, AI stands as a crucial ally in modernizing pediatric cancer care.
The Role of Collaborative Research in Pediatric Oncology
Collaborative research plays a vital role in advancing the field of pediatric oncology, fostering innovations that can lead to improved outcomes for young patients. Studies involving multiple institutions enable researchers to pool diverse data sources, enhancing the power and reliability of findings. For instance, the collaboration between Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center has led to significant advancements in the use of AI for predicting pediatric cancer relapse through thorough data analysis.
By working together, institutions can tackle the complexities of pediatric cancers more effectively, while also sharing expertise that paves the way for future developments. This spirit of collaboration can accelerate the translation of research into clinical application, which is critical for implementing innovative strategies such as AI-driven risk prediction models into everyday clinical practice, ultimately benefiting patients and their families.
Investing in Future Technologies for Pediatric Cancer Treatment
Investment in future technologies targeting pediatric cancer treatment is crucial. With the rapid advancement of AI capabilities and novel therapeutic technologies, funding initiatives can significantly enhance research opportunities. Investing in AI-driven tools specifically designed to analyze pediatric oncology datasets has the potential to refine our understanding of cancer processes and patient outcomes.
The benefits of such investments extend beyond mere research; they bring hope for more effective treatment protocols tailored for specific patient needs. As technologies like temporal learning and advanced imaging continue to develop, their implementation can lead to breakthroughs in early detection and intervention strategies, fundamentally altering the trajectory of pediatric cancer care.
Potential Impact of AI on Pediatric Cancer Survivors
The advancements in AI technologies bear profound implications not just for active patients but also for pediatric cancer survivors. By improving the accuracy of relapse predictions, AI can help ensure that survivors are monitored appropriately and receive timely interventions should any signs of recurrence appear. This careful surveillance can provide peace of mind for families who often grapple with the long-term impacts of cancer in children’s lives.
Furthermore, the insights generated from AI analyses contribute to a deeper understanding of late effects and quality of life issues that survivors face. By focusing on individual outcomes and tailoring follow-up care based on predictive analytics, the healthcare system can better support pediatric cancer survivors in their journey towards recovery, leading to improved survivorship outcomes and overall well-being.
Frequently Asked Questions
What is pediatric cancer relapse prediction and why is it important?
Pediatric cancer relapse prediction refers to the use of advanced methods, including AI and MRI imaging, to assess the likelihood of cancer returning in children. This is crucial for tailoring follow-up care, as many pediatric cancers, such as gliomas, can be successfully treated, but relapses can lead to severe consequences. Better prediction models enable earlier interventions and optimized treatment plans.
How does AI enhance pediatric cancer relapse prediction compared to traditional methods?
AI significantly improves pediatric cancer relapse prediction by analyzing multiple MRI scans over time, utilizing temporal learning techniques. Unlike traditional methods which rely on single images, AI identifies subtle changes across a patient’s imaging history to predict relapse more accurately, achieving up to 89% accuracy in some cases.
What role does MRI imaging play in predicting relapse in pediatric oncology?
MRI imaging is vital in pediatric oncology for monitoring brain tumors such as gliomas. Advances in AI have enabled the analysis of sequential MRI scans, enhancing the ability to predict cancer relapse by recognizing patterns of change over time that may indicate an increased risk of recurrence.
Can temporal learning be applied in other areas of pediatric cancer treatment?
Yes, temporal learning principles used in pediatric cancer relapse prediction can be adapted to other areas in pediatric oncology that require longitudinal imaging, such as monitoring treatment efficacy or predicting complications. This innovative approach may revolutionize care across various cancer types.
What were the findings of the recent study on AI in pediatric cancer relapse prediction?
The study revealed that an AI model utilizing temporal learning could predict the recurrence of pediatric gliomas with 75-89% accuracy within one year post-treatment. This marked improvement over traditional methods underscores the potential for AI tools to revolutionize how pediatric oncology manages follow-up care.
How does the prediction model for brain tumor recurrence help in clinical settings?
The prediction model for brain tumor recurrence aids clinicians by stratifying patients based on their risk levels. This enables them to tailor follow-up imaging schedules and initiate preventive treatments for high-risk patients, potentially improving long-term outcomes for children recovering from brain tumors.
What future implications does AI in pediatric cancer relapse prediction hold for treatment plans?
The implications of AI in pediatric cancer relapse prediction are vast, including the potential to reduce unnecessary imaging in low-risk patients and implement early interventions for those identified as high-risk. This personalized approach could enhance the overall effectiveness of treatment plans in pediatric oncology.
| Key Point | Details |
|---|---|
| AI Tool for Relapse Prediction | An AI tool was developed to predict the risk of relapse in pediatric cancer patients more accurately than traditional methods. |
| Study Scope | The study analyzed nearly 4,000 MRI scans from 715 pediatric patients. |
| Temporal Learning Technique | Researchers used temporal learning to train the AI model with multiple scans taken over time. |
| Prediction Accuracy | The AI achieved a prediction accuracy of 75-89% for recurrence, vastly improved from 50% accuracy of single image analyses. |
| Potential Clinical Applications | Researchers aim to use AI predictions to reduce unnecessary imaging and target adjuvant treatments for high-risk patients. |
Summary
Pediatric cancer relapse prediction has been significantly advanced by the use of innovative AI tools, which outperform traditional methods. This breakthrough in technology not only offers hope for more accurate risk assessments in young patients but also promises to improve their quality of care by minimizing stress related to extensive imaging procedures. As research continues, there is potential for this AI approach to transform clinical practices in managing pediatric cancer effectively.
Pediatric Brain Cancer Prediction Using AI for Better Outcomes
Pediatric brain cancer prediction is revolutionizing the way we approach the diagnosis and management of childhood brain tumors. Recent advancements in artificial intelligence (AI) technology have shown promise in significantly enhancing the accuracy of predicting cancer recurrence, particularly in cases of pediatric gliomas. A groundbreaking study highlighted the efficacy of a novel AI tool, which leverages temporal learning to analyze multiple MRI scans over time, offering a more precise assessment of relapse risk than traditional methods. This innovative approach not only aids in earlier detection but also aims to reduce the psychological burden on young patients and their families. As researchers delve deeper into pediatric cancer research, the integration of AI in medicine emerges as a beacon of hope for improving outcomes in vulnerable populations.
The prediction of brain cancer in children, particularly regarding the likelihood of recurrence, has become a critical area of focus within the medical community. Utilizing cutting-edge technology and methodologies, experts are exploring the implications of artificial intelligence in analyzing longitudinal imaging data for pediatric tumors. By harnessing advanced algorithms to monitor changes in brain scans over time, researchers can develop more accurate forecasts for conditions like pediatric gliomas. This shift toward predictive analytics not only enhances patient care but also contributes significantly to the evolving landscape of pediatric cancer treatment strategies. As investigations continue, the promise of improved diagnostics and targeted interventions draws nearer, bolstering hope for affected families.
The Role of AI in Predicting Pediatric Brain Cancer Recurrence
In recent years, AI technology has significantly transformed the landscape of medical diagnosis and treatment, particularly in pediatric oncology. The latest advances in AI algorithms have demonstrated a superior ability to predict relapse risk in pediatric brain cancer patients compared to traditional methods. Specifically, a study conducted by researchers at Mass General Brigham highlighted the effectiveness of a temporal learning AI tool that analyzed brain scans over time, providing a more nuanced understanding of pediatric gliomas. This innovative approach allows clinicians to identify patients who might be at greater risk for recurrence, thus tailoring follow-up care more effectively.
The AI model developed in the study utilizes a technique called temporal learning, which synthesizes data from various MR scans taken over a span of months after surgery. By looking at sequences of images rather than isolated scans, this model has achieved an impressive accuracy rate of 75-89% in predicting relapse risks for low or high-grade gliomas. This not only changes how pediatric brain cancer is monitored but also paves the way for potential breakthroughs in pediatric cancer research, enabling better-informed decision-making in clinical settings.
Improving Care for Pediatric Glioma Patients
The care management of pediatric glioma patients is undergoing a significant shift thanks to advancements in predictive analytics and AI technologies. Traditionally, children diagnosed with brain tumors have faced the anxiety of regular imaging follow-ups, a routine that can often be burdensome for both the children and their families. However, by adopting AI tools that predict the likelihood of cancer recurrence, healthcare providers may soon alleviate some of this stress. For instance, children determined to be at lower risk could potentially reduce the frequency of their imaging sessions, allowing them to focus more on recovery and less on medical appointments.
Moreover, the integration of AI in medicine highlights an essential shift toward personalized treatment strategies. With the ability to identify patients more likely to experience recurrence early, oncologists can initiate targeted adjuvant therapies proactively. This is especially crucial in the case of pediatric brain cancer, where timely intervention can make a significant difference in outcomes. As research continues to validate the efficacy of these AI models, the ultimate goal is to enhance the care continuum for young patients fighting pediatric cancer.
Furthermore, the cross-institutional collaboration exhibited in this study underscores the importance of joint efforts in the field of pediatric cancer research. By pooling resources and data, institutions like Boston Children’s Hospital and Dana-Farber are setting a precedent for how interdisciplinary partnerships can drive advancements in cancer care.
Temporal Learning AI: A Game Changer for Pediatric Oncology
Temporal learning AI represents a groundbreaking advancement in how brain imaging data is utilized in the field of pediatric oncology. Unlike conventional AI methods that rely on individual images to generate predictions, temporal learning provides a comprehensive analysis by interpreting sequences of scans over time. This innovative application is particularly pertinent in assessing pediatric gliomas, which typically require ongoing monitoring following treatment. The study underscored how this AI tool could effectively track subtle changes in patients’ conditions, greatly improving the accuracy of relapse predictions.
Researchers have noted that the integration of temporal learning into standard imaging protocols could lead to more precise evaluations of disease progression. By being able to analyze a series of scans, physicians can gain insight into the treatment efficacy and make informed decisions regarding treatment adjustments. This method not only enhances the reliability of predictions regarding recurrence but also signifies a move towards a more adaptive model of care that can respond dynamically to each patient’s journey.
The Future of AI in Pediatric Cancer Research
As the field of pediatric cancer research continues to evolve, the role of AI is becoming increasingly critical. The ability to harness vast amounts of imaging data and learn from it offers hospitals and research institutions the opportunity to dramatically change treatment protocols for young cancer patients. The insights gained from studies like the one at Mass General Brigham provide a foundation for future investigations into how AI can be used to predict outcomes in various types of pediatric malignancies, not just gliomas.
Furthermore, ongoing research in AI applications may uncover novel patterns in pediatric cancer recurrence, advancing our understanding of tumor biology. The potential for AI-driven tools to assist in early diagnosis, personalized medicine, and treatment effectiveness monitoring could revolutionize care in pediatric oncology, leading to improved outcomes for patients. This transition towards data-driven solutions represents a pivotal step that harnesses technology to better serve the needs of children battling cancer.
Challenges and Considerations in AI Implementation
While the potential benefits of AI in predicting pediatric brain cancer recurrence are significant, several challenges remain in the implementation of these tools in clinical settings. One of the primary concerns is ensuring the accuracy of AI predictions across diverse patient populations and varying healthcare infrastructures. As the initial studies have shown promising results, further validation across different clinical settings is essential for the wider adoption of AI technologies. This will involve addressing variability in scans, diverse healthcare access, and patient demographics.
Moreover, ethical considerations around privacy and data security must be prioritized. As AI systems require vast amounts of patient data for training, ensuring that this information is used responsibly and securely is paramount. Stakeholders in pediatric cancer research, including hospitals, regulatory agencies, and patient advocates, must collaborate to establish clear guidelines that prioritize patient safety while promoting technological advancement in treatment methodologies.
Pediatric Gliomas: Understanding Relapse Risks
Pediatric gliomas, while often treatable, pose a significant challenge due to the uncertain risk of recurrence. Understanding these risks is vital to providing effective treatment plans and managing patient care. Traditionally, the assessment of relapse risk has relied on a combination of histological analysis and imaging studies, but these methods have not always provided clear forecasts. The incorporation of AI predictive tools allows for a more nuanced evaluation of individual cases, potentially leading to improved risk stratification.
Researchers emphasize the need for ongoing studies to further explore the variances in glioma behavior among pediatric patients. Factors such as tumor location, genetic markers, and patient age can all influence the likelihood of recurrence. By integrating AI analysis into these investigations, the hope is to uncover deeper insights that could guide more personalized treatment strategies for young patients facing the challenges of brain cancer.
The Impact of AI on Patient Monitoring Practices
The advent of advanced AI tools in medical imaging is quantifiably reshaping the methodologies used in monitoring pediatric cancer patients post-treatment. With traditional imaging follow-up protocols often being resource-intensive and stressful for young patients, AI-enhanced monitoring represents a paradigm shift. By utilizing predictive analytics that assess multiple scans over time, clinicians can better gauge patient conditions without subjecting them to unnecessary anxiety.
This new approach not only has the potential to reduce the frequency of MRI scans for patients at lower risk of recurrence but could also streamline workflows in busy pediatric oncology departments. With quicker and more reliable analyses, healthcare teams can focus on providing care that is more responsive and tailored to each patient’s unique situation. The outcome of these innovations could herald a new era in pediatric cancer care, where patient experience and treatment efficacy are significantly enhanced.
Collaborative Efforts in Pediatric Cancer Research
The collaboration among various institutions, such as Mass General Brigham, Boston Children’s Hospital, and Dana-Farber, underscores the importance of collective efforts in advancing pediatric cancer research. These partnerships not only enable the pooling of resources but also facilitate the sharing of diverse expertise that can lead to innovative breakthroughs in understanding and treating pediatric gliomas. Such integrative research approaches are essential for tackling the complexities associated with pediatric malignancies.
Going forward, fostering inter-institutional collaborations will be crucial for accelerating research efforts aimed at understanding the prognosis of pediatric brain cancers. These alliances can yield larger datasets and enhanced study designs, which in turn can inform the development of AI tools tailored to identifying recurrence risks. Ultimately, these cooperative efforts may be instrumental in improving treatment outcomes and survival rates for affected children.
Future Directions and Innovations in Pediatric Oncology
Looking ahead, the integration of AI into pediatric oncology is poised to propel forward not only research but also clinical application. With emerging technologies continually reshaping diagnostic frameworks, there is a pressing need to adapt treatment protocols accordingly. The promise of AI-driven insights into pediatric brain cancer, particularly through refined understanding of gliomas, holds transformative potential for patient care.
Continued investment in research and development surrounding AI tools will be essential for harnessing their full capacity in predictive medicine. As studies validate the accuracy and effectiveness of these innovations, we can expect to see a ripple effect throughout pediatric cancer management practices, fostering a climate of hope and resilience for young patients and their families.
Frequently Asked Questions
How does pediatric brain cancer prediction using AI improve outcomes for glioma patients?
Pediatric brain cancer prediction utilizing AI enhances outcomes by accurately assessing the risk of recurrence in glioma patients. The AI tool analyzes multiple brain scans over time, employing a technique called temporal learning to identify subtle changes that indicate potential relapses, thus allowing for more proactive treatment approaches.
What advancements in pediatric cancer research have stemmed from AI in medicine regarding gliomas?
Advancements in pediatric cancer research, particularly in pediatric gliomas, have been significantly influenced by AI in medicine. This includes the development of robust predictive models that leverage temporal learning, enabling clinicians to forecast cancer recurrence with improved accuracy, ultimately informing treatment decisions and reducing unnecessary stress for families.
What is temporal learning AI and how does it apply to pediatric brain cancer prediction?
Temporal learning AI is a machine learning technique that sequentially analyzes multiple imaging data points over time. In pediatric brain cancer prediction, it allows the AI to recognize trends and changes across several MRI scans post-surgery, leading to a more dependable assessment of relapse risk in patients with brain tumors like gliomas.
What findings did the study on pediatric gliomas reveal about predicting brain cancer recurrence?
The study revealed that the AI model could predict brain cancer recurrence in pediatric gliomas with an accuracy of 75-89%, compared to 50% accuracy from traditional methods based on single images. This highlights the importance of using multiple scans to improve prediction reliability.
Why is predicting brain cancer recurrence important in pediatric patients?
Predicting brain cancer recurrence in pediatric patients is crucial because it enables timely intervention and personalized treatment strategies. By accurately forecasting who is at risk, healthcare providers can tailor follow-up care, minimize unnecessary stress on patients and families, and optimize outcomes for children battling pediatric gliomas.
How can AI tools change the landscape of follow-up care in pediatric brain cancer treatment?
AI tools can revolutionize follow-up care by reducing the frequency of imaging for low-risk pediatric brain cancer patients while ensuring that high-risk patients receive timely and targeted therapies. This shifts the emphasis from routine scans to risk-based personalized care, improving both the experience and outcomes for pediatric patients.
What role does artificial intelligence play in enhancing accuracy for pediatric brain cancer prediction?
Artificial intelligence enhances accuracy in pediatric brain cancer prediction through advanced analytical capabilities, such as identifying patterns in longitudinal imaging data. This results in better identification of at-risk patients and allows for more effective, individualized treatment planning.
| Key Points |
|---|
| An AI tool developed to predict relapse risk in pediatric patients with brain cancer has shown improved accuracy compared to traditional methods. |
| The study emphasizes the importance of early identification of relapse risk in children with gliomas to enhance patient care. |
| Temporal learning technique was used in AI to analyze multiple MRI scans over time, significantly improving predictive capabilities. |
| Results indicate a prediction accuracy of 75-89% for glioma recurrence within one year post-treatment. |
| Further validation and clinical trials are necessary to implement AI predictions in routine care. |
Summary
Pediatric brain cancer prediction is significantly enhanced through the use of AI technology, as shown in a recent study by researchers at Mass General Brigham. The study highlighted that an AI model utilizing temporal learning achieved a remarkable accuracy rate of 75-89% in predicting the risk of relapse in children with gliomas, surpassing traditional single-scan methods. This advancement indicates the potential for better monitoring and early intervention in pediatric patients, ultimately aiming to improve their long-term health outcomes.
Research Grants in Public Health: Securing Vital Funding
Research grants in public health play a pivotal role in shaping the landscape of health advancements, enabling scientists to explore critical issues such as cancer risk reduction research and nutrition. These grants, often funded by federal research funding agencies like the NIH, not only empower researchers but also foster innovation in public health research. To succeed in this competitive field, understanding effective grant writing strategies is essential, as applications must demonstrate the potential impact of proposed studies. Despite the challenges, successful grants can lead to groundbreaking projects that significantly enhance public health and safety. As researchers navigate the NIH funding process, their efforts ultimately aim to create healthier communities and improve lives.
In the realm of health and wellness, funding opportunities for scientific inquiries are essential, particularly in disciplines focused on community well-being and disease prevention. Federal funding support, often termed as research grants, enables scholars to embark on pivotal studies aimed at confronting pressing public health challenges. When health scientists engage in extensive grant writing, they not only seek financial backing but also ensure their projects align with national health priorities. This intricate funding ecosystem involves rigorous evaluation processes, such as the NIH funding review, which emphasizes the significance and innovation of each application. By securing these necessary resources, researchers can uncover transformative insights that contribute to the greater good of society.
The Importance of Federal Research Funding in Public Health
Federal research funding is the backbone of innovation in public health. It empowers researchers to conduct studies that have the potential to save lives and improve the overall health of communities. Grants from agencies like the National Institutes of Health (NIH) not only provide financial support but also boost the credibility of research endeavors. With these resources, public health researchers, like Karen Emmons and Jorge Chavarro, can focus on critical issues such as cancer risk reduction and nutritional impacts on human health. This funding allows for comprehensive studies that address pressing health disparities and pave the way for new public health strategies.
The NIH funding process embodies a rigorous evaluation system, which ensures that only the most innovative and proven research ideas receive grants. This system promotes a competitive atmosphere where scientists are encouraged to explore fresh avenues and collaborate with community partners. As Emmons highlights, preparing a grant proposal involves significant groundwork, including establishing relationships with various stakeholders. The overall goal of this federal funding is to not only advance scientific knowledge but also to have tangible impacts on public health, ultimately leading to healthier populations.
Effective Grant Writing Strategies for Public Health Researchers
Writing a successful grant application is essential for researchers seeking federal research funding, and it requires strategic planning and careful consideration. Public health researchers must ensure that their proposals clearly demonstrate the significance and innovation of their research ideas. According to Chavarro, a vital component of the proposal is the specific aims page, which outlines the study’s objectives, its potential impact, and evidence supporting the proposed methodologies. Being concise yet comprehensive is key; each line must resonate with the reviewers, justifying the need for funding and establishing the research’s relevance.
Additionally, researchers must be acutely aware of the competitive nature of grant applications. Site visits, collaborations, and preliminary results can enhance the proposal’s strength but require thorough preparation and patience. Emmons emphasizes the importance of staying informed about recent academic publications and trends, as this knowledge allows researchers to position their work responsively. Understanding the nuances of the NIH funding process, such as the necessity for ethical considerations and budget validation, further enhances the chances of securing grants in public health.
Navigating Challenges in Public Health Research Funding
Despite the crucial role that federal funding plays, public health researchers frequently encounter challenges when pursuing grants. As highlighted in recent reports, significant political factors can lead to the freezing of research grants, hindering progress in vital studies. For example, the interruption of Harvard’s funding due to administrative decisions depicts how external influences can obstruct crucial public health research initiatives. Researchers like Emmons and Chavarro face uncertainties that stem from these political dynamics, which weaken their ability to conduct essential studies that address health issues such as cancers and chronic diseases.
Moreover, the competitive landscape of grant submissions means that not all well-prepared applications will receive funding. With success rates often hovering around 14% for major grants like the NIH R01, the pressure to produce high-quality and groundbreaking research increases for scientists. Researchers often need to resubmit their proposals after receiving feedback, requiring them to adapt and refine their ideas, which can be both a tedious and time-consuming process. The evolving nature of public health challenges necessitates that researchers remain resilient and persistent in their quest for funding opportunities.
The Role of Collaboration in Securing Research Grants
Collaboration among researchers, academic institutions, and community partners is essential for securing federal research funding. Emmons emphasizes the significance of forming partnerships with community organizations when implementing research that targets underserved populations. These collaborations can foster a comprehensive understanding of community needs and enhance the relevance of research proposals. By showcasing engagement with community stakeholders in grant applications, researchers can demonstrate a commitment to improving public health outcomes, which is favorable in the eyes of funding agencies.
Additionally, networking with other researchers can provide insights and strategies for successful grant applications. Chavarro’s participation in scientific review groups enables him to see the intricacies of successful proposals, which he can then apply to his own work. These interactions build a supportive environment where researchers can share advice on navigating the grant writing process, ultimately increasing their chances of securing funding. Collaboration not only enriches the research experience but also strengthens the scientific community’s ability to address public health challenges effectively.
Innovative Research Methods in Cancer Risk Reduction
As the field of public health evolves, innovative research methods are essential for understanding and reducing cancer risks. Emmons, for instance, focuses on incorporating community feedback in her research to develop studies that specifically target cancer prevention in underserved demographics. This approach not only enhances the impact of her work but also aligns with federal funding priorities that emphasize health equity and community engagement. By utilizing innovative methods that incorporate real-world data and community involvement, she increases the likelihood of securing grants that address these critical public health issues.
Furthermore, employing cutting-edge technologies and tools can augment cancer risk reduction research. By leveraging advancements in genomics and data analytics, researchers can identify high-risk populations and tailor prevention strategies accordingly. These innovative approaches enhance the robustness of grant applications, presenting funding agencies with compelling evidence of the research’s potential for significant public health impact. With the growing emphasis on personalized medicine and targeted interventions, integrating such methodologies is crucial for obtaining competitive federal research funding.
The Impact of Funding on Health Outcomes
Securing federal funding has far-reaching implications for public health outcomes. Financial support from federal agencies allows researchers to conduct long-term studies that can lead to breakthroughs in disease prevention and treatment. As demonstrated by Emmons and Chavarro’s work, effective research can lead to practical applications, such as new public health policies or community health interventions aimed at reducing cancer rates. The link between federal research funding and improved health outcomes is critical, emphasizing the need for continued investment in public health research.
Moreover, the economic impact of successful research funded by federal grants cannot be understated. By focusing on health issues such as cancer, researchers contribute not only to individual health but also to the broader economy by reducing healthcare costs and increasing workforce productivity. The insights gained from well-funded studies can shape public health initiatives and inform governmental policies, enhancing community health and leading to societal benefits. Consequently, the significance of obtaining federal research funding extends beyond academia, reaching into the lives of individuals and communities.
Future Directions in Public Health Research Funding
The landscape of public health research funding is continually evolving, necessitating adaptability from researchers pursuing federal grants. An increased focus on health disparities, particularly influenced by recent global health crises, presents new avenues for research and funding opportunities. As agencies like the NIH recalibrate their funding strategies, public health researchers should remain agile, aligning their proposals with emerging public health priorities such as equity in healthcare access, preventative measures, and response strategies to health crises.
Looking towards the future, public health researchers must also leverage technology in proposal writing and project execution. Digital tools for data collection and analysis, as well as platforms for virtual collaboration, can enhance research efficiency and outreach. Integrating these technologies within research proposals not only strengthens their design but also aligns with the increasing emphasis on innovation in the funding process. As researchers proactively adapt to these changes, they will be better positioned to secure the necessary funding to drive impactful public health research forward.
Assessment and Feedback in Grant Writing
The process of assessment and feedback is integral to the success of grant applications in public health research. After submitting proposals, researchers often receive critiques that can guide subsequent submissions, providing valuable insights into improving their ideas and methodologies. Both Emmons and Chavarro emphasize the necessity of being receptive to feedback, as it allows researchers to refine their proposals, making them more competitive in future funding opportunities. This cycle of continuous improvement is essential for advancing research efficacy and ensuring alignment with funding agency expectations.
Moreover, engaging with peers during the grant writing process can enhance the overall quality of applications. Whether it’s through collaborative team discussions or informal workshops, sharing drafts and receiving constructive criticism enriches grant proposals and fosters an environment of collective growth within the scientific community. By prioritizing assessment and feedback, public health researchers can navigate the complexities of the grant writing process more effectively, thereby increasing their likelihood of securing the crucial federal funding needed for impactful health initiatives.
Frequently Asked Questions
What are the key components of grant writing strategies for public health research?
Grant writing strategies for public health research typically include conducting a thorough literature review, identifying funding sources such as federal research funding opportunities, creating a compelling narrative for the proposal, detailing innovative methodologies, and establishing partnerships with community organizations. Researchers must also ensure that their projects address specific public health needs and are evidence-based to increase their chances of success.
How can federal research funding support cancer risk reduction research?
Federal research funding plays a crucial role in cancer risk reduction research by providing resources needed for innovative studies, pilot testing, and community engagement. Grants from agencies like the National Institutes of Health (NIH) facilitate projects aimed at understanding cancer prevention strategies, identifying at-risk populations, and implementing effective outreach programs tailored to underserved communities.
What is the NIH funding process for public health research?
The NIH funding process for public health research involves several stages, starting with the submission of a grant proposal that outlines the research aims, significance, and methodology. Proposals undergo a rigorous peer review process, where Scientific Review Groups evaluate their innovation and relevance to public health. Only the highest-scoring applications receive funding, ensuring that resources support impactful research.
How can researchers improve their chances of receiving public health research grants?
Researchers can improve their chances of receiving public health research grants by building strong collaborative networks, staying updated on current trends and publications, crafting clear and specific research aims, and thoroughly justifying budget requests. Engaging with community partners can also strengthen proposals by demonstrating the potential for real-world impact.
What challenges do researchers face when applying for federal research funding in public health?
Researchers applying for federal research funding in public health face challenges such as a competitive grant landscape, the need for comprehensive proposals that meet stringent guidelines, and the escalating costs of innovative research. Additionally, navigating the detailed NIH requirements and addressing feedback from previous applications can be time-consuming and complex.
What are the benefits of securing federal grants for public health research?
Securing federal grants for public health research offers several benefits, including access to significant funding that supports important health initiatives, the ability to conduct innovative studies that can lead to breakthroughs in health policy and practices, and opportunities for researchers to collaborate with public and private sectors. Ultimately, these grants enable researchers to make meaningful contributions to improving population health.
| Key Points |
|---|
| Karen Emmons and Jorge Chavarro are prominent researchers in public health, focusing on cancer prevention and nutrition, respectively. |
| Securing federal grants is crucial for research endeavors, impacting studies related to health and wellness. |
| Challenges have arisen due to funding freezes, particularly from the Trump administration, affecting various research projects. |
| Grant applications involve rigorous preparation, including extensive planning, ethical considerations, and detailed budgeting. |
| Success rates for grant proposals can be low; for instance, the NCI’s latest success rate is only 14.6%. |
| Feedback from unsuccessful applications allows researchers to improve and resubmit their proposals. |
| Public-private partnerships are highlighted as essential for maintaining a commitment to science as a public good. |
Summary
Research grants in public health are vital for advancing knowledge and developing effective health solutions. The competitive nature of obtaining these grants, as illustrated by the experiences of researchers like Karen Emmons and Jorge Chavarro, underscores the dedication required to secure funding amid challenges. The support from federal grants not only facilitates innovative research but also ensures that public health initiatives can thrive and respond to pressing health issues, ultimately benefiting society at large.

Alzheimer’s Research Unveils New Treatments and Discoveries
Alzheimer’s research is at the forefront of a critical battle against one of the most challenging neurodegenerative diseases facing our aging population today. Notably, the groundbreaking work of neuroscientist Beth Stevens at the Stevens Lab highlights the pivotal role of microglial cells as essential components of the brain’s immune system. These cells are responsible for monitoring brain health, and their malfunction can significantly impact cognitive functions, leading to conditions like Alzheimer’s disease. By investigating how aberrant pruning affects neuronal connections, Stevens aims to uncover new pathways for finding Alzheimer’s treatment that can potentially revolutionize care for the millions affected. As the need for effective interventions grows, her research not only enhances our understanding of Alzheimer’s but also paves the way towards developing innovative solutions that could change lives.
The quest for understanding Alzheimer’s disease has evolved into a major scientific endeavor, spotlighting the critical roles played by specialized brain cells known as microglia. These cells act as guardians of the brain, resembling a robust immune system that reacts to various ailments and injuries. Researchers, including celebrated scientist Beth Stevens, are delving into the ways these cells can either protect the brain or contribute to the progression of neurodegenerative disorders. By illuminating the relationship between microglial activity and cognitive decline, this line of inquiry is fostering fresh perspectives on identifying potential treatments and early detection methods for Alzheimer’s and related conditions. The implications of such research are vast, promising new hope for future generations impacted by these devastating diseases.
Understanding Microglial Cells and Their Role in Alzheimer’s Research
Microglial cells are essential components of the brain’s immune system, functioning similarly to the body’s first line of defense against external threats. In the context of Alzheimer’s research, these cells play a vital role in maintaining neuronal health. They constantly monitor the brain environment, ready to respond to injury or infection. However, recent studies spearheaded by researchers like Beth Stevens have revealed that microglia can also contribute to neurodegenerative diseases when their pruning processes go awry. This aberrant pruning can lead to the mismanagement of synaptic connections, which is critical in conditions such as Alzheimer’s disease, Huntington’s disease, and other forms of dementia.
Stevens’ groundbreaking findings highlight how a deeper understanding of microglial behavior could lead to innovative therapies aimed at modulating these brain immune cells. By targeting the mechanisms that govern microglial activity, scientists hope to develop interventions that restore normal function and prevent the onset of Alzheimer’s disease. The implications of such research are profound as they may pave the way for earlier detection and treatment of neurodegenerative diseases, ultimately improving the quality of life for millions of individuals affected by such disorders.
The Intersection of Basic Science and Alzheimer’s Treatment
The journey into Alzheimer’s treatment often begins with foundational research in basic science. Researchers like Beth Stevens emphasize that exploring the intricate workings of microglial cells and their role within the brain can seem distant from clinical applications at first. However, this basic science provides critical insights that fuel advancements in treatment options. Stevens’ lab investigates how these brain immune cells sculpt synapses during development, leading to discoveries that unravel the complexities surrounding neurodegenerative diseases. This research not only enhances our understanding but also serves as a stepping stone for finding Alzheimer’s treatment.
Moreover, robust funding from federal agencies, notably the National Institutes of Health (NIH), has been pivotal in supporting these exploratory studies. Without such backing, many groundbreaking findings might have remained undiscovered. The translation of knowledge gained from basic science to therapeutic strategies is not linear, yet each revelation pushes science forward, indicating that today’s curiosity-driven research will be the foundation for tomorrow’s breakthroughs in Alzheimer’s diagnosis and treatment.
Implications of Aging Population on Alzheimer’s Disease
As the U.S. population continues to age, the incidence of Alzheimer’s disease is predicted to rise dramatically, with estimates indicating that the number of affected individuals may double by 2050. This impending increase poses significant challenges not only for healthcare systems but also for families impacted by the disease. With projections indicating that associated healthcare costs could soar from $360 billion to a staggering $1 trillion, it is imperative to prioritize research and treatment strategies aimed at combating Alzheimer’s disease. Understanding the role of microglial cells in this context becomes increasingly relevant, as scientists seek to develop effective interventions.
Investing in Alzheimer’s research and related neurodegenerative studies is not just about treating the disease; it is about alleviating the burden on caregivers and improving outcomes for patients. Innovative advances like those led by Beth Stevens demonstrate the potential to change the narrative around Alzheimer’s disease, moving from a prognosis of cognitive decline to a future where effective treatments are available. This shift is crucial for maintaining the dignity and quality of life for millions of Americans facing this diagnosis.
Beth Stevens: Pioneering Research in Neurodegenerative Disease
Beth Stevens has emerged as a leading figure in the field of Alzheimer’s research through her innovative studies on microglial cells. Her work has significantly shifted the understanding of how these brain immune cells function and their critical role in maintaining neurological health. Stevens posits that while microglia serve essential functions in clearing debris and modulating synaptic connections during brain development, their dysregulation can contribute to the etiology of neurodegenerative diseases. This duality in function highlights the importance of her research and the potential pathways for therapeutic interventions.
Recognized as a MacArthur “genius” for her contributions, Stevens embodies the spirit of curiosity-driven science. She underscores the interconnectedness of seemingly disparate research areas, showing how fundamental studies can lead to real-world applications in treating diseases like Alzheimer’s. By illuminating the role of microglia, Stevens and her team at Boston Children’s Hospital and the Broad Institute are not just contributing to academic knowledge; they are creating pathways towards finding Alzheimer’s treatment and improving the lives of those battling neurodegenerative disorders.
Neurodegenerative Diseases: Understanding the Pathways
Neurodegenerative diseases encompass a range of disorders characterized by gradual degeneration of the nervous system, leading to cognitive decline and physical impairments. Conditions like Alzheimer’s, Parkinson’s, and Huntington’s disease fundamentally challenge our understanding of brain function and longevity. As researchers delve into these diseases, microglial cells emerge as key players, responding to the neuronal environment and influencing the progression of neurodegeneration. This relationship between microglia and neurodegenerative diseases invites further exploration to uncover potential biomarkers and treatment strategies.
By dissecting the intricate pathways involved in neurodegenerative diseases, scientists can develop targeted therapies that address the root causes of these disorders. Insights gleaned from studies on microglial function can provide valuable information on how to modulate neuroinflammation and protect neuronal integrity. The research being championed by Stevens and others signifies a shift towards precision medicine in neurodegenerative conditions, where interventions are tailored to individual patient profiles, ultimately leading to more effective outcomes.
The Importance of Biomarkers in Alzheimer’s Research
Biomarkers play a critical role in the early detection and management of Alzheimer’s disease, allowing for intervention before significant cognitive decline occurs. Identifying reliable biomarkers can enhance our understanding of disease progression and improve patient outcomes. Research led by Beth Stevens underscores how microglial activity can serve as a potential biomarker for Alzheimer’s disease and other neurodegenerative disorders. By examining the behavior of these brain immune cells, scientists hope to create diagnostic tools that facilitate earlier detection of Alzheimer’s.
However, the journey to establishing effective biomarkers is fraught with challenges. Scientists must ensure that these markers accurately reflect the disease’s underlying pathology and are measurable through practical means, such as blood tests or imaging techniques. The exploration of microglial-related biomarkers represents a promising avenue of research that could revolutionize Alzheimer’s diagnosis and lead to timely therapeutic interventions. As advancements continue, the hope is that early detection through biomarkers will play a vital role in combating the rising tide of Alzheimer’s disease in an aging population.
Innovations in Treatment for Alzheimer’s Disease
The landscape of Alzheimer’s treatment is evolving rapidly, fueled by innovative research and emerging technologies. Advances in understanding microglial cells have opened new avenues for developing therapeutic strategies that address the neuroinflammatory processes underlying the disease. Researchers are pursuing various approaches, including small molecules, monoclonal antibodies, and immunotherapies, that target microglial function to restore balance in the brain’s immune response. Stevens’ work exemplifies the potential of such innovations as she investigates ways to modulate microglial activity for more effective Alzheimer’s treatments.
As scientific inquiry continues to unravel the complexities of Alzheimer’s disease, a richer understanding of its mechanisms leads to more comprehensive treatment options. By bridging the gap between fundamental research and clinical application, scientists are better equipped to tackle the various forms of Alzheimer’s and other neurodegenerative diseases. Innovative treatment approaches inspired by foundational studies on microglial cells may provide much-needed hope for millions affected by cognitive decline, shifting the outcome of Alzheimer’s from inevitability to possibility of improved health and quality of life.
The Future of Alzheimer’s Research: Collaborative Efforts
Collaboration continues to be a cornerstone in the fight against Alzheimer’s disease, bringing together scientists, clinicians, and policymakers to address this multifaceted challenge. Research initiatives that unite various disciplines can pave the way for breakthroughs in understanding the pathophysiology of Alzheimer’s. Accelerating discoveries necessitate not only collaboration among researchers but also partnerships with organizations committed to funding Alzheimer’s research. As demonstrated by Beth Stevens’ work, collaboration enhances the potential for significant findings that will ultimately transform clinical practices.
Looking ahead, it is crucial to foster a culture of collaboration across the scientific community, where sharing insights and resources can lead to more accelerated progress in Alzheimer’s research. By focusing on partnerships that leverage diverse expertise, researchers can develop more holistic approaches to tackling this complex disease. The future of Alzheimer’s research relies heavily on the synergistic efforts of dedicated scientists who are committed to better understanding this debilitating condition and translating that knowledge into effective interventions and treatments.
Frequently Asked Questions
What role do microglial cells play in Alzheimer’s research?
Microglial cells are essential components of the brain’s immune system and play a crucial role in Alzheimer’s research. They help maintain brain health by clearing dead or damaged cells and pruning synapses. However, dysregulation of these processes can contribute to neurodegenerative diseases, including Alzheimer’s. Understanding their functions is key in finding Alzheimer’s treatment.
How are neurodegenerative diseases like Alzheimer’s linked to abnormalities in microglial cells?
Research indicates that abnormalities in microglial cells can exacerbate neurodegenerative diseases such as Alzheimer’s. These cells are responsible for monitoring brain health, and improper pruning of synapses may lead to the progression of Alzheimer’s disease. Investigating these links is vital for developing new strategies in Alzheimer’s research.
What insights has Beth Stevens provided in the field of Alzheimer’s research?
Beth Stevens has made significant contributions to Alzheimer’s research by highlighting the importance of microglial cells in the brain’s immune system. Her studies demonstrate that these cells can significantly influence neurodegenerative diseases by improperly pruning synapses, underscoring the potential for new treatments and early detection biomarkers in combating Alzheimer’s.
Why is understanding the brain’s immune system critical in finding Alzheimer’s treatments?
Understanding the brain’s immune system, particularly the role of microglial cells, is critical in finding Alzheimer’s treatments. These cells help regulate brain health and detect damage. Disruptions in their function are linked to Alzheimer’s and other neurodegenerative diseases, indicating that targeting these immune responses could lead to groundbreaking therapies.
What future advancements can we expect in Alzheimer’s research based on recent findings?
Recent advancements from researchers like Beth Stevens have opened avenues for new medications and biomarkers for Alzheimer’s disease. As we uncover more about the role of microglial cells in the pathology of Alzheimer’s, we can anticipate more effective treatments that could significantly improve the quality of life for those affected by this neurodegenerative disease.
How does federal funding influence Alzheimer’s research and findings like those from Beth Stevens?
Federal funding plays an instrumental role in Alzheimer’s research, providing critical resources for scientists like Beth Stevens. Her foundational studies on microglial cells were largely supported by grants from agencies like the NIH, which foster curiosity-driven research that can lead to significant breakthroughs in understanding and treating Alzheimer’s disease.
| Key Component | Details |
|---|---|
| Research Focus | Investigates the role of microglial cells in Alzheimer’s disease and other neurodegenerative disorders. |
| Significant Discovery | Aberrant pruning by microglia can contribute to conditions like Alzheimer’s and Huntington’s disease. |
| Research Institution | Stevens Lab, Boston Children’s Hospital and Broad Institute of MIT and Harvard. |
| Impact on Treatment | Developing new medicines and biomarkers for earlier detection of Alzheimer’s. |
| Future Outlook | As the U.S. population ages, the number of Alzheimer’s cases is expected to double by 2050. |
| Funding Source | Majority of funding is from federal agencies like NIH, supporting foundational and curiosity-driven science. |
| Recognition | Beth Stevens recognized as a MacArthur ‘genius’ for her pioneering research in 2015. |
Summary
Alzheimer’s research is crucial in understanding and combating one of the most significant health crises of our time. The work led by Beth Stevens highlights how microglial cells can influence neurodegeneration through their pruning processes. By leveraging foundational science, Stevens’ lab is paving the way for innovative treatments and earlier detection of Alzheimer’s disease, which currently affects millions of Americans. As we approach a future with a doubling of Alzheimer’s cases, the implications of such research are profound, emphasizing the need for continuous support and exploration in this vital field.

Global Health: Atul Gawande’s Urgent Call for Action
Global health is a pressing concern that affects millions of people worldwide, and recent insights from figures such as Atul Gawande shed light on its critical state. As the former leader of USAID’s Bureau for Global Health, Gawande highlights the detrimental impacts following the dismantling of vital health programs and the public health infrastructure that supports them. Without robust global health initiatives, the fight against diseases like HIV, tuberculosis, and malaria is severely compromised, threatening the lives of vulnerable populations. The consequences of government policies on health underscore the urgent need for renewed investment and commitment to health systems worldwide. Understanding these dynamics is essential for fostering effective USAID health programs that can lead to meaningful change and better health outcomes for all.
The term ‘international wellness’ encompasses various aspects of how health is managed and prioritized across the globe. In his discussions, Atul Gawande emphasizes the ramifications of fluctuating policies on health systems and the importance of maintaining a strong public health framework. The decline of critical health initiatives has far-reaching consequences, especially in low-income countries where resources are scarce. As leaders in global health navigate these challenges, the call for effective health interventions remains louder than ever. By exploring the interconnectedness of health policies and community well-being, we can better understand the imperative for sustained global health efforts.
The Impact of Dismantling Global Health Initiatives
The dismantling of the U.S. Agency for International Development (USAID) and its global health initiatives has created a significant void in public health infrastructure. As Atul Gawande highlighted, the removal of dedicated staff and crucial programs has resulted in devastating consequences for populations relying on American support. The termination of more than 85 percent of USAID programs has not only affected millions of individuals but has also diminished the U.S.’s standing as a leader in global health outreach. Without these critical structures in place, efforts to combat diseases and improve health outcomes in underserved communities are severely hampered.
Furthermore, the impact of these changes can be seen in the immediate response to health crises. For instance, thanks to USAID’s previous work, emergency response times to outbreaks like Ebola were significantly reduced, allowing for prompt intervention in affected areas. However, the current state reflects a worrying trend where federal support and research funding for health initiatives are under constant threat. Citizens in both domestic and international contexts feel the repercussions, highlighting the urgent need for robust public health infrastructure that can withstand political shifts.
The Role of Government Policies in Health Outcomes
Government policies play a crucial role in shaping health outcomes at both national and global levels. As Gawande implied, recent actions, including funding freezes at key health institutions like the National Institutes of Health and the Centers for Disease Control, threaten the backbone of public health in the U.S. These policies directly affect research programs that have historically contributed to significant advancements in areas such as maternal health, childhood mortality, and infectious diseases. Consequently, weakened governmental support can lead to increased mortality and morbidity rates, particularly in vulnerable populations.
Moreover, effective public health policies are essential for fostering collaboration between agencies, universities, and medical centers. Gawande’s reflection on the role of USAID emphasizes the importance of ongoing partnerships and the follow-through beyond merely implementing health solutions. Consistent government backing can elevate vaccination rates and improve health systems in ways that save lives. However, as the political landscape shifts, so too does the assurance of sustained commitment to health initiatives, creating uncertainty among health experts and the communities they serve.
Innovations in Global Health Programs
Despite the setbacks faced by initiatives like USAID, the global health community remains hopeful for the future. Atul Gawande’s tenure at USAID was marked by innovative programs aimed at addressing pressing health challenges, particularly in maternal and child health. For example, prior to his departure, the agency was poised to introduce a low-cost treatment package that significantly mitigated severe postpartum hemorrhaging—a leading cause of maternal deaths worldwide. These innovations are crucial as they not only address immediate healthcare needs but also help in building sustainable health systems in low and middle-income countries.
Additionally, innovations fostered through partnerships with organizations such as the World Health Organization illustrate the ongoing commitment to improving health outcomes globally. By utilizing technical assistance and implementing evidence-based practices, vaccination rates and healthcare efficiency can dramatically increase, creating long-lasting impacts. The engagement of health experts in these innovative processes is vital for ensuring that communities have access to effective healthcare solutions, even amidst broader geopolitical challenges.
The Future of Public Health Infrastructure
The future of public health infrastructure hangs in the balance, especially in light of the challenges highlighted by Gawande. The commitment to restore and preserve USAID’s capabilities will require concerted efforts from leaders in health and policy. Currently, the dismantling threatens the critical frameworks established over decades to support health initiatives globally. Without investing in the rebuilding of infrastructure, the health of millions hangs precariously, placing increased emphasis on the role of state and local governments to step up.
Looking forward, it is essential for stakeholders, including governmental agencies, public health advocates, and the private sector, to collaborate in revitalizing the public health framework. The mutual benefits of a well-resourced public health sector are evident—not only in terms of immediate health responses but also in promoting long-term economic stability and community well-being. As Gawande has passionately articulated, the fight for a strong public health infrastructure is critical, and all hands must be on deck to ensure a healthier future for all.
Educational Initiatives in Health Sciences
Education plays a pivotal role in fortifying public health infrastructure. As Atul Gawande pointed out during his address, the engagement of students and faculty in scientific inquiry and public health is vital for ongoing progress. Empowering future healthcare leaders through robust educational programs not only equips them with essential skills but also nurtures a generation that is informed and ready to tackle global health challenges. Investing in health education serves as a proactive approach to ensure that individuals can contribute positively in times of health crises.
Moreover, collaborations between educational institutions and health agencies can bridge the gap between theoretical knowledge and practical application. Programs that link students with real-world health initiatives—such as those historically facilitated by USAID—can enhance their learning experience while simultaneously benefiting communities. As Gawande emphasized, the expertise of healthcare professionals will be invaluable regardless of the shifting political winds, highlighting the need for continual investment in health education.
Community Engagement in Global Health Solutions
Community engagement is essential for the success of global health initiatives. Gawande’s remarks about the importance of health systems working closely with individuals at the ground level emphasize the need for tailoring health interventions to meet actual community needs. When communities are actively involved in the planning and implementation of health programs, the likelihood of achieving positive outcomes increases significantly. Engagement fosters trust, facilitates open communication, and incorporates local knowledge into solutions, making efforts more effective and sustainable.
Furthermore, community-based health programs can address unique health challenges that different populations face. With the right support, local organizations can gather data, identify health trends, and tailor programs that fit the cultural and social dynamics of the communities they serve. For instance, outreach efforts related to maternal health and childhood diseases can benefit tremendously from local insights, ensuring that interventions are not just imposed but co-developed. This participatory approach is fundamental for driving long-term health improvements and fostering resilience against future health crises.
The Interconnection of Global Health and Economic Stability
The relationship between global health and economic stability is undeniable. Atul Gawande’s reflections on the broader impact of USAID’s initiatives illustrate how health policies not only improve lives but also strengthen economies. Healthy populations are more productive, which in turn fosters economic growth and stability. When public health funding is cut, the resulting deterioration in health outcomes affects workforce productivity, healthcare costs, and ultimately, economic performance. Thus, investments in global health should be viewed as critical economic strategies.
Aligning health initiatives with economic policies ensures that health remains a priority in government agendas. As the global community recovers from the repercussions of recent policy shifts, emphasizing the interconnectedness of health and economic prosperity will be pivotal. For example, programs that improve maternal and child health not only save lives but also lead to better educational outcomes and economic opportunities for future generations. A comprehensive understanding of these interconnections can guide more effective public policies aimed at promoting overall societal well-being.
Leveraging Data for Health Improvements
Leveraging data is a crucial aspect of developing effective global health strategies. Gawande’s account of USAID’s innovative approaches to disease surveillance showcases the role data plays in mitigating health threats. The organization enhanced response times to outbreaks through real-time data collection, which empowered policymakers to act swiftly and effectively. By utilizing data analytics, health organizations can identify trends, allocate resources wisely, and monitor the efficacy of interventions.
Moreover, access to data facilitates transparency and accountability in health initiatives. It allows stakeholders, including governments, NGOs, and communities, to evaluate the success of health programs and make informed decisions moving forward. Emphasizing data-driven approaches in public health can assure communities that their needs are being prioritized while also fostering trust in governmental and global health initiatives. As emphasized by Gawande, a commitment to using data to shape health policies will be essential in addressing future challenges effectively.
The Importance of Science and Medicine in Health Discourse
As Atul Gawande emphasized, the importance of science and medicine in shaping public health discourse cannot be overstated. In an era marked by misinformation and skepticism toward expertise, advocating for science-based solutions is crucial for the advancement of global health. Engaging with communities about the value of scientific research and medicine can cultivate trust and encourage compliance with public health guidelines, ultimately leading to better health outcomes.
Additionally, the ongoing efforts to uphold the integrity of scientific inquiry in the face of political interference are essential. Gawande’s remarks about federal funding freezes signal a troubling trajectory for research and progress in healthcare. Strengthening public discourse around the significance of sustained investment in science will be necessary to ensure that research-backed policies are prioritized in health decision-making, reinforcing the longstanding role of science as a pillar in global health.
Frequently Asked Questions
What are some key global health initiatives impacting at-risk populations?
Several global health initiatives focus on improving health outcomes for at-risk populations. These initiatives, often supported by organizations like USAID, include maternal and child health programs that prevent deaths and enhance access to essential health services. Innovative programs target diseases such as HIV, tuberculosis, and malaria, significantly increasing survival rates and quality of life for millions.
How has Atul Gawande influenced USAID health programs?
Atul Gawande has had a significant impact on USAID health programs through his leadership in improving public health infrastructure. His focus on data-driven health initiatives has streamlined emergency response to outbreaks and enhanced maternal health services, benefiting millions globally. Gawande’s advocacy for robust health policies has brought attention to the need for sustainable global health solutions.
What challenges does global health face due to government policies?
Government policies can greatly influence global health by either supporting or undermining public health infrastructure. Recent policy shifts, including staffing cuts at USAID, have posed challenges to initiatives aimed at disease prevention and health promotion. Such changes can disrupt long-term investments in health programs that are vital for safeguarding vulnerable populations.
How does USAID contribute to strengthening global health infrastructure?
USAID plays a crucial role in strengthening global health infrastructure by funding and implementing programs that improve healthcare access, disease surveillance, and crisis response. Through collaborations with governments and local organizations, USAID enhances capabilities to tackle public health challenges, streamline vaccination efforts, and ensure healthier outcomes for communities worldwide.
What is the impact of government funding on global health initiatives?
Government funding is essential for the success of global health initiatives. Adequate financial support allows organizations like USAID to develop and sustain programs that address critical health issues, from maternal and child health to infectious disease control. Cuts in funding can hinder progress, reduce service delivery, and escalate health challenges in low-income regions.
Why is public health infrastructure important for global health?
Public health infrastructure is vital for global health as it ensures effective disease prevention, response to health emergencies, and the delivery of essential health services. A robust infrastructure supports research, enhances healthcare access, and facilitates coordination during outbreaks. Investing in public health strengthens the ability to address emerging global health threats and improve overall population health.
What role does USAID play in maternal and child health globally?
USAID is a leader in global maternal and child health initiatives, providing funding, technical assistance, and advocacy to reduce mortality rates. Their programs focus on improving prenatal care, skilled birth attendance, and access to necessary medical interventions. By supporting these initiatives, USAID contributes significantly to extending life expectancies for women and children worldwide.
How does the impact of USAID’s health programs vary across different countries?
The impact of USAID’s health programs varies widely depending on local contexts, healthcare systems, and existing public health challenges. In countries with strong governmental support and existing infrastructure, USAID’s initiatives can lead to rapid improvements in health outcomes. Conversely, in regions facing political instability or resource shortages, the effectiveness of these programs may be diminished, underscoring the need for tailored approaches.
| Key Point | Details |
|---|---|
| Effects of USAID Cuts | The dismantling of USAID has led to the termination of over 85% of its programs, harming millions globally. |
| Global Health Impact | USAID previously played a critical role in surveilling diseases and improving health outcomes for maternal and child health. |
| Future of Global Health Leadership | Gawande expressed uncertainty about the U.S.’s role in leading global health but noted other countries may take on more responsibility. |
| Call to Action | Despite the challenges, Gawande urged students and faculty to remain committed to science and medicine. |
Summary
Global health is at a critical intersection, underscored by Atul Gawande’s account of the devastating effects of USAID’s dismantling. The extensive cuts to international health programs have not only impacted millions of lives globally but also jeopardized the U.S.’s ability to lead in this field. Gawande emphasizes the need for a renewed commitment to health and science infrastructure. As new leaders emerge, the importance of maintaining robust global health initiatives remains imperative for the future of public health around the world.

Global Flourishing: Insights on Youth Well-Being and Happiness
Global flourishing is a comprehensive concept that encompasses the well-being of individuals and communities across diverse contexts. A recent mental health study led by Harvard researchers has uncovered significant insights into the state of youth well-being, revealing that financial stability alone does not determine happiness or success in life. This comprehensive study highlights the importance of spiritual well-being, meaningful relationships, and character development as critical facets of human flourishing. With economic development taking center stage in many global discussions, it becomes crucial to balance financial growth with initiatives that support mental health and youth engagement. Addressing these dimensions not only impacts individual lives but can lead to a more harmonious and thriving society.
The pursuit of global prosperity extends beyond mere economic metrics; it is an exploration of human potential and community vitality. By looking at well-being from multiple angles, including emotional health, social engagement, and life purpose, we begin to understand the intricate dynamics that foster a flourishing existence. The recent research underscores the need to advocate for holistic support for young people, illuminating the role of both psychological and spiritual wellness in their development. It emphasizes that national advancement should be measured not only in wealth but also in the quality of life and relationships fostered among citizens. Ultimately, promoting a comprehensive approach to youth fulfillment can pave the way for sustainable global progress.
The Importance of Youth Well-Being in Global Flourishing
Youth well-being is a critical component of global flourishing, as highlighted by the findings of a major mental health study. As economic development continues to rise in numerous nations, it has become increasingly clear that financial wealth does not equate to the flourishing of youth. In fact, the Global Flourishing Study revealed that middle-income countries often outperform wealthier nations in metrics related to youth mental health and happiness. This discrepancy raises pressing questions regarding the investments societies are making in the mental health resources available to young populations.
Furthermore, the focus on youth well-being is essential, not only for individual satisfaction but also for the societal fabric as a whole. Young people represent the future, and their experiences with mental health, relationships, and spiritual well-being significantly influence their ability to contribute positively to their communities. Therefore, fostering environments that support youth well-being should be a top priority for policymakers to ensure a thriving global society.
Spiritual Well-Being as a Factor in Flourishing
Spiritual well-being has been identified as a significant variable in defining human flourishing. The Global Flourishing Study collected data that suggests participation in religious activities and community involvement can dramatically enhance life satisfaction and mental health among individuals. This correlation underscores the notion that spiritual practices foster connections and a sense of purpose, which are crucial for overall well-being. In many cases, individuals who engage in regular spiritual practices report higher levels of emotional resilience and happiness.
Moreover, the implications of spiritual well-being extend beyond the individual to societal levels. Communities that cultivate a strong sense of spiritual connectivity often experience greater social cohesion, compassion, and support for one another. As highlighted in the study, there is a need for integration of spiritual dimensions in discussions surrounding economic development and policy-making, as neglecting this aspect can hinder both individual flourishing and community health.
Economic Development and Youth Flourishing: A Complex Relationship
The relationship between economic development and youth flourishing presents a complex landscape, challenging conventional wisdom that wealth automatically leads to happiness. The findings from the Global Flourishing Study suggest that, in many cases, financial prosperity does not guarantee fulfilling lives for younger generations. For instance, countries like Indonesia, which may be classified as middle-income, often demonstrate higher levels of youth well-being compared to wealthier countries such as Japan. This raises critical questions about the nature of contemporary economic development and its effects on mental health among youth.
It is essential to evaluate how economic policies can be designed to support the holistic development of youth, rather than solely focusing on capital accumulation. This includes investments in mental health resources, educational frameworks that promote character development, and community programs that foster positive relationships. By aligning economic initiatives with the broader goals of human flourishing, societies can create environments where young people not only survive but thrive, ultimately contributing to overall societal progress.
Key Findings of the Global Flourishing Study
The Global Flourishing Study represents a monumental effort to disaggregate the concept of well-being into measurable variables such as happiness, health, and character. With a sample size of around 203,000 participants from diverse backgrounds, the study provides comprehensive insights into what contributes to human flourishing across various cultures. Among its many findings, the study emphasizes the importance of relational dynamics and character traits in determining overall life satisfaction, particularly among youth.
Another significant finding is the critical role of early childhood experiences in shaping adult flourishing. Survey results indicate that positive maternal and paternal relationships, as well as good health during childhood, correlate strongly with higher levels of flourishing in adulthood. Such insights highlight the necessity for early intervention programs that focus on mental health support for families, thereby paving the way for better outcomes for future generations.
The Shifting Landscape of Mental Health Among Youth
Recent trends indicate a concerning shift in mental health patterns among youth, with the flourishing metrics showing declines compared to older generations. According to the Global Flourishing Study, the once U-shaped curve of life satisfaction has morphed into a J-shape, where youth experience relative stagnation in flourishing levels before reporting improvements in later decades. This shift signals a need for urgent attention to the issues faced by adolescents and young adults today, including mental health challenges and the pressures of societal expectations.
Addressing these emerging mental health issues requires a multifaceted approach, integrating academic, personal, and community support systems that prioritize mental wellness. Encouraging mindfulness practices, promoting open conversations about mental health struggles, and enhancing spiritual well-being could be instrumental in helping youth navigate these critical years. Through collective efforts, we can foster a supportive landscape where young people can thrive.
The Role of Community in Enhancing Flourishing
Communities play a pivotal role in enhancing the well-being and flourishing of their members, particularly the youth. The Global Flourishing Study indicates that strong social ties and a sense of belonging are intricately linked to happiness and overall life satisfaction. Communities that prioritize building connections among residents often see significant benefits in collective mental health and character traits, making them essential for supporting youth well-being.
Local initiatives that promote community engagement, volunteerism, and cooperative activities can help foster positive relationships and a sense of purpose among young individuals. For instance, programs that encourage youth participation in community service or conflict resolution projects can cultivate character development and spiritual well-being. By empowering young people to contribute to their communities, we can enhance not only their personal flourishing but also the overall health of society.
Investing in a Flourishing Future: Policy Implications
The findings from the Global Flourishing Study raise critical considerations regarding policy initiatives aimed at youth well-being. Evidence suggests that current economic models often fail to account for essential aspects of flourishing, such as spiritual well-being and meaningful relationships. Thus, decision-makers must re-evaluate their strategies to ensure that investments in youth are made with a holistic understanding of what promotes true flourishing beyond financial success.
Policies should focus on integrating mental health resources in schools, enhancing community-based programs, and offering support for nurturing family environments, all of which serve to uplift youth well-being. As we consider the future, it is imperative that governments and organizations work collaboratively to create a framework where young people’s needs are prioritized, ultimately aiming for a future where every young person has the opportunity to flourish.
The Relationship Between Happiness and Financial Security
Understanding the relationship between happiness and financial security is crucial in discussions about youth well-being. Findings from the Global Flourishing Study reinforce the idea that economic stability alone does not guarantee happiness. In fact, the study highlighted that lower-income countries often exhibit higher levels of happiness among youth compared to some wealthier nations, challenging the common belief that financial prosperity equates to a flourishing life.
Moreover, the nuances of financial security extend beyond just job stability or income level. Factors such as cost of living, community support systems, and access to mental health resources play significant roles in determining overall well-being. As a society, paying attention to multifaceted approaches to financial security can create environments where youth feel both secure and fulfilled, leading to higher levels of flourishing.
Understanding Character Development in Global Flourishing
Character development is a crucial aspect of the Global Flourishing Study, highlighting its role in fostering a meaningful and fulfilling life. The surveys suggest that traits such as empathy, resilience, and integrity significantly contribute to overall happiness and well-being. For youth, developing these character traits not only enhances their individual flourishing but also nurtures healthier community dynamics, showing that the cultivation of character can have a ripple effect throughout society.
Programs that emphasize character education within schools and community organizations are essential for equipping young people with the tools needed to navigate challenges while maintaining meaningful relationships. By investing in character development initiatives, societies can promote enduring well-being that transcends financial measures, ultimately leading to a more integrated approach to human flourishing.
Frequently Asked Questions
How does global flourishing relate to youth well-being and mental health?
Global flourishing incorporates various dimensions of youth well-being, including mental health. Studies show that when youth experience high levels of flourishing, they are more likely to report better mental health outcomes, reduced anxiety, and overall life satisfaction. Investing in programs that promote positive relationships, character, and spiritual well-being can enhance youth flourishing and improve their mental health.
What role does economic development play in global flourishing?
Economic development is often associated with improvements in material wealth, yet the Global Flourishing Study suggests that financial circumstances alone do not guarantee flourishing. Countries that prioritize social connections, community support, and spiritual fulfillment tend to rank higher in flourishing, indicating that holistic approaches to economic development that include these factors are crucial for societal well-being.
Why is spiritual well-being essential for human flourishing on a global scale?
Spiritual well-being is a key component of human flourishing, as it fosters a sense of purpose, community, and connection beyond material success. The Global Flourishing Study finds that individuals who frequently engage in spiritual or religious practices report higher levels of overall flourishing, integrating meaning and relationships into their lives, thus supporting the argument that spiritual pathways are vital for comprehensive global well-being.
How can we improve youth well-being in the context of global flourishing?
Improving youth well-being within the framework of global flourishing can be achieved through education, mental health resources, and community programs that focus on developing strong relationships, enhancing character, and fostering a sense of purpose. Policymaking should prioritize these areas to create environments that nurture youth flourishing and combat the alarming trends of decreased well-being among younger generations.
What findings about flourishing were revealed in global studies of mental health?
Global studies on mental health, such as the Global Flourishing Study, reveal concerning trends regarding youth flourishing, particularly in developed nations like the U.S. The studies show a shift in flourishing patterns and highlight that youth today face unique challenges that affect their mental health, suggesting a need for targeted interventions and increased investments in youth-focused flourishing programs.
| Key Points | Details |
|---|---|
| Global Study Findings | A major study on human flourishing indicates youth well-being concerns, particularly in the U.S., showcasing that wealth does not guarantee happiness. |
| Survey Depth | Involving 203,000 participants across 22 countries, the survey explored health, happiness, meaning, relationships, financial security, and more. |
| Flourishing Metrics | Youth flourishing has dropped from a U-shaped curve to a J-shaped curve, indicating significant concerns about young adults’ well-being. |
| Financial vs. Social Well-being | Indonesia ranks highest in flourishing despite being lower-income, while Japan (richer) scored low in relational metrics. |
| Future Implications | The study raises questions on investing in youth and balancing economic development with spiritual and relational needs. |
Summary
Global flourishing is dependent on more than just economic status; it encompasses health, relationships, and a sense of purpose. This major study reveals the critical need to invest in the youth to enhance their well-being and happiness. By understanding the factors that contribute to individual and collective flourishing, we can guide societies towards ensuring that future generations thrive economically, socially, and spiritually.

Medical Research Safety: The Impact of Funding Cuts
Medical research safety is a crucial aspect of advancing healthcare, ensuring that patients who participate in clinical trials are protected from potential risks. As funding cuts from federal sources threaten research initiatives, the oversight provided by Institutional Review Boards (IRBs) becomes even more vital. These boards play a key role in safeguarding participant rights and welfare by reviewing research proposals for ethical compliance and monitoring ongoing studies for adherence to established safety protocols. With challenges such as the NIH funding impact and bureaucratic hurdles, the integrity of patient safety in research hangs in the balance. The commitment to maintaining ethical standards in medical research is paramount for fostering public trust and enhancing the quality of clinical trials.
In the realm of healthcare innovation, the protection of individuals involved in scientific inquiries is often referred to as research participant safety. The integrity of clinical trials is upheld through meticulous scrutiny by regulatory bodies, particularly Institutional Review Boards (IRBs), which ensure that ethical guidelines are followed throughout the research process. With recent developments, including drastic funding limitations, concerns regarding oversight efficiency have escalated, underlining the significance of ethical review in safeguarding participant well-being. As various institutions face challenges associated with NIH funding cuts and the demands of maintaining clinical trials ethics, the welfare of research subjects remains a priority. The collaborative efforts of professionals in this field are essential to navigate these complexities and ensure that advancements in medical research can proceed without compromising patient safety.
Impact of NIH Funding on Patient Safety in Research
The National Institutes of Health (NIH) plays a pivotal role in fostering patient safety within clinical research. The funding dispensed by the NIH not only facilitates groundbreaking studies but is also crucial for the maintenance of strict oversight through Institutional Review Boards (IRBs). This oversight ensures compliance with ethical standards, protecting participants from potential risks associated with experimental treatments. Without adequate NIH funding, the operational capabilities of IRBs may diminish, leading to a lapse in the thorough review processes that shield patients from harm. Furthermore, NIH funding allows for the training and support essential for research personnel in navigating ethical dilemmas, making it indispensable for the safety of human subjects.
Moreover, NIH funding cuts have broader implications for patient safety during clinical trials. When funding is halted, as seen with the recent suspension affecting Harvard’s research initiatives, ongoing studies may face interruptions. These interruptions not only delay findings that could potentially benefit patients but also risk further eroding public trust in the research community. The perception of research as a safe and ethical endeavor hinges on robust oversight mechanisms funded by the NIH, underscoring the critical nature of continued federal support in safeguarding the health of research participants.
The Role of IRB Oversight in Clinical Trials
Institutional Review Boards (IRBs) are integral to protecting patient safety in clinical trials. They act as regulatory bodies that conduct thorough reviews of research proposals to evaluate ethical considerations and ensure informed consent. The meticulous process adopted by IRBs examines various factors such as study design, recruitment strategies, and risk assessments. These protocols are indispensable in upholding the integrity of clinical research and the safety of participants. Without IRB oversight, studies risk deviating from established ethical norms, potentially endangering the well-being of those participating in clinical trials.
Furthermore, the impact of funding cuts on IRB operations cannot be understated. As financial support wanes, many IRBs may struggle to maintain their rigorous standards, leading to inadequate protection for study participants. The consequence is particularly severe for multisite studies, which rely heavily on IRB coordination to manage compliance across diverse locations. Federal funding is essential to keep these oversight processes robust and effective, ensuring that the ethical obligations towards patient safety are met consistently across all research initiatives.
Ethics of Clinical Trials: Historical Context
The ethical scrutiny surrounding clinical trials has evolved significantly in response to historical injustices. Events such as the Tuskegee Syphilis Study and unethical practices during World War II have highlighted the necessity for stringent ethical oversight in medical research. The establishment of IRBs was a direct response to these violations, seeking to protect the rights and welfare of human subjects. Understanding this history is vital for contemporary researchers and regulatory bodies, as it reinforces the importance of patient consent and transparency in research practices. It also serves as a reminder of the potential for abuse in clinical research, underscoring the continued need for vigilance in ethical considerations.
The evolution of ethics in clinical trials illustrates the dynamic nature of research practices responding to societal values and lessons learned from past failures. By fostering an ethical framework grounded in respect for patient rights and safety, the research community can restore public confidence in clinical trials. Ensuring that IRBs are adequately funded and supported is crucial for maintaining these ethical standards and preventing a return to the troubling practices of the past.
Funding Cuts and Their Impact on Research Integrity
Funding cuts, such as those imposed on the SMART IRB contract, pose a significant threat to the integrity of medical research. The ability to secure continuous funding is essential not just for carrying out studies but also for maintaining the ethical oversight needed to protect participants. When funding is reduced, researchers may face pressures to expedite their work, potentially compromising ethical standards in the process. Such a scenario directly impacts patient safety, as the thorough review and monitoring processes essential to safeguard participants may become diluted or halted altogether.
Additionally, funding challenges can lead to increased competition among institutions for limited research dollars, potentially resulting in shortcuts in patient safety protocols. With a “publish or perish” culture dominating academia, the emphasis may shift from ethical research practices to achieving rapid results. This shift can undermine the trust placed in clinical trials by patients and the public, further complicating efforts to engage communities in research participation. The sustainability of ethically sound research practices hinges on the support and resources allocated to maintain robust funding for oversight and safety processes.
Public Trust in Medical Research: Reinforcing Patient Safety
Public trust is a cornerstone of successful clinical research, emphasizing the need for transparency and ethical conduct. When patients feel confident that their participation in research is safeguarded by regulatory bodies, they are more likely to engage in clinical trials. This trust is fostered through clear communication regarding the purpose, risks, and benefits of research participation, often mediated by IRBs. By providing a layer of protection and ethical oversight, IRBs not only enhance patient safety but also serve to build public confidence in the research process.
However, the trust can quickly erode in the face of funding cuts and halted research projects. When studies are disrupted or fail to meet ethical standards due to lack of resources, it sends a negative signal to potential participants. The potential for harm and public skepticism may deter individuals from volunteering for future studies, hindering the advancement of medical research. Therefore, maintaining robust funding for ethical oversight is imperative to reinforce public trust and ensure the safety of patients in medical research.
Restoring Funding: A Path for Future Research
Efforts to restore funding for vital research initiatives, such as those overseen by SMART IRB, are crucial for the future of clinical studies. The continual flow of federal funds enables research institutions to uphold high standards of ethics and safety in patient care. By advocating for increased NIH funding and public support, researchers can work to mitigate the effects of previous cuts and recommit to safeguarding the health of study participants. Collaborative efforts across institutions can drive this agenda forward, promoting a research environment that prioritizes participant safety and integrity.
Moreover, restoring funding is not solely about navigating financial constraints; it is also about investing in the ethical foundations of research. Stakeholders must come together to emphasize the importance of patient safety and the ethical obligations of researchers. By ensuring that IRBs remain adequately funded and staffed, the research community can solidify its commitment to ethical oversight. This, in turn, encourages volunteers to participate in research studies, which is essential for advancing medical discoveries and improving public health outcomes.
Challenges of Multi-Site Studies Under Funding Cuts
Multi-site studies present unique challenges in the realm of clinical research, particularly in light of recent funding cuts. These studies often necessitate collaboration between multiple institutions, which relies heavily on efficient IRB processes to review and manage ethical compliance across diverse sites. Without sufficient funding, the capability to execute these reviews may diminish, leading to delays in participant recruitment and potential compromises in patient safety. The halt in new clinical site additions due to funding disruptions not only stifles research progress but also places undue strain on existing studies, threatening the integrity of the data collected and the well-being of participants.
Additionally, the complexity of managing multi-site collaborations requires robust support and resources to ensure ethical oversight. Each participating site must adhere to uniform standards for patient safety, which necessitates effective communication and training facilitated by well-funded IRBs. Without these resources, the risk of ethical inconsistencies increases, potentially causing harm to participants and undermining public confidence in clinical research. For the continued success of multi-site studies, it is essential that funding be reinstated to support the infrastructure necessary for maintaining high ethical standards.
Investing in Research to Safeguard Public Health
Investing in medical research is crucial for the future of public health. Adequate funding not only supports the development of innovations that can lead to groundbreaking treatments but also ensures that the safety and rights of participants are actively prioritized. By bolstering the financial resources available for research oversight, governments and institutions can foster an environment where ethical conduct and patient safety thrive. Continued investment in ethical research practices is imperative to protect participants and enhance the overall quality of medical studies, thus advancing public health.
In the face of challenges posed by funding cuts, it is critical that stakeholders advocate for the importance of sustained investment in research. By highlighting success stories that stem from well-funded initiatives and the vital role of IRBs in protecting patient safety, advocates can make a compelling case for increasing financial support. Ultimately, prioritizing resources for medical research not only benefits participants but also contributes to the wider societal goal of improving health outcomes for all.
Frequently Asked Questions
How do NIH funding impacts patient safety in medical research?
NIH funding plays a crucial role in supporting research that involves human participants, ensuring thorough review and oversight by Institutional Review Boards (IRBs). These funds allow for compliance with safety regulations, ethical standards, and participant protections, ultimately enhancing patient safety in medical research.
What is the role of IRB oversight in safeguarding patients in clinical trials?
IRB oversight is essential for protecting patients in clinical trials. These boards meticulously review study proposals to assess risks, ensure informed consent, and monitor participant welfare, acting as a necessary checks-and-balances system in the ethical conduct of medical research.
How can research funding cuts affect patient safety in clinical trials?
Cuts to research funding can disrupt ongoing studies and IRB operations, endangering patient safety by halting critical research, delaying ethical reviews, and diminishing oversight resources which are vital for protecting participants involved in clinical trials.
Why is patient safety a major concern in medical research funding?
Patient safety is paramount in medical research funding because financial support facilitates comprehensive ethical reviews by IRBs, ensuring that patients are well-informed, that risks are appropriately managed, and that studies adhere to strict safety protocols.
What are the consequences of halted medical research on patient safety?
Halted medical research can lead to increased risks for patients already enrolled in studies, delays in important clinical findings, and a general erosion of public trust in the research community, ultimately compromising patient safety in clinical trials.
How does the SMART IRB system enhance patient safety in multi-site studies?
The SMART IRB system simplifies the oversight process for multi-site studies by providing a uniform review process that ensures participant protections are uniformly applied, thus enhancing patient safety across diverse research locations.
In what ways does clinical trials ethics impact patient safety?
Clinical trials ethics directly impact patient safety by establishing essential guidelines for informed consent, risk assessment, and participant monitoring, which are necessary to safeguard the rights and well-being of individuals involved in medical research.
What historical events have shaped the current focus on patient safety in medical research?
Historical events, such as the unethical Tuskegee Syphilis Study and the Willowbrook hepatitis experiments, have prompted the establishment of ethical standards and regulations to enhance patient safety, shaping today’s robust IRB oversight requirements in medical research.
| Key Point | Details |
|---|---|
| Funding Disruption | The Trump administration’s freezing of over $2 billion in federal research grants to Harvard has halted various medical research efforts. |
| Impact on Patient Safety | The halt in funding has adversely affected the rights and safety of patients participating in medical studies. |
| Role of IRBs | Institutional Review Boards (IRBs) ensure compliance with regulations and protect research participants’ rights and welfare. |
| Historical Context | Past instances of unethical research highlight the need for stringent oversight and ethical standards, established partly by IRB functions. |
| Consequences of Funding Cuts | Ongoing studies are at risk, as funding cuts hinder the ability to safely manage and monitor research, potentially harming participants. |
Summary
Medical research safety is a critical concern, especially in light of the recent disruptions caused by significant funding cuts. The freezing of federal research grants has halted vital safety initiatives within medical research, putting the welfare of patient participants at risk. It is essential for continued support and oversight to ensure ethical standards and protect those involved in medical studies, highlighting the importance of funding in maintaining the integrity and safety of research practices.

CRISPR Technology: The Ethics Behind Gene Editing
CRISPR technology is revolutionizing the field of gene editing, offering unprecedented capabilities to manipulate genetic material in pursuit of curing diseases. This powerful tool can precisely alter genes to eliminate ailments such as sickle cell anemia, raising important questions about the implications of such changes. As researchers examine the potential for CRISPR to reshape human health, they must also grapple with the ethics of gene editing and the broader societal impact on health equity. The conversation surrounding the latest in biomedical ethics emphasizes not just the science, but also the responsibility that comes with such potent capabilities. Amidst the promise of advanced treatments, the ongoing debate reflects the tension between innovation and the moral considerations that must guide these scientific breakthroughs.
Gene editing, particularly through advanced techniques like CRISPR, represents a frontier in modern medicine, holding the key to potentially eradicating genetic disorders. This groundbreaking technology allows scientists to tailor genetic sequences with precision, sparking discussions about its ethical dimensions and the ramifications for health equity in diverse communities. The term ‘genetic modification’ encapsulates the ongoing discourse about our ability and responsibility to alter human genetics, especially in cases like the treatment of sickle cell disease. As stakeholders in the medical field ponder the implications of these advancements, they must navigate complex issues related to biomedical ethics and the potential societal divide created by access to such innovative therapies. In exploring these themes, it becomes clear that the future of gene editing is as much about moral choices as it is about scientific progress.
Understanding CRISPR Technology in Gene Editing
CRISPR technology represents a revolutionary advancement in the field of gene editing, providing scientists with tools to modify the DNA of living organisms with unprecedented precision. This innovative system was initially derived from a bacterial immune response, allowing researchers to target specific sequences within the genome. By utilizing CRISPR’s RNA-guided mechanism, scholars can now cut out faulty genes and insert correct versions, opening the door to potential cures for genetic disorders such as sickle cell anemia. Moreover, the implications of such technology extend beyond mere correction; they raise significant questions about the essence of genetic modification and its ethical ramifications.
As CRISPR technology continues to evolve, it emphasizes the need to address both the scientific and ethical concerns that accompany gene editing. The capability to eliminate devastating genetic diseases is undoubtedly appealing; however, it prompts a broader dialogue about the boundaries of genetic intervention. For instance, what are the responsibilities of researchers and clinicians in deciding which traits to alter? With possibilities for germline editing, decisions made today could affect generations to come, raising concerns over unintended consequences and ethical considerations surrounding health equity and access.
Ethics of Gene Editing and Health Equity
The ethics of gene editing are at the forefront of discussions regarding CRISPR technology and its applications. As highlighted in Neal Baer’s talk, one key ethical concern is the potential for socioeconomic disparities to widen if such technologies become available only to those who can afford them. For instance, the sickle cell treatment currently costs around $2.2 million, creating questions about who truly benefits from these advancements. The disparity in access to cutting-edge biomedical technology not only poses challenges for affected populations but also raises fundamental issues of justice and health equity in medical practice.
Moreover, as gene editing techniques continue to become more refined, the ethical landscape expands to encompass diverse issues, from the potential for designer babies to the implications of editing health-related traits versus non-pathological human variations. The discussion encourages a holistic approach to biomedical ethics, urging policymakers and the scientific community to consider the broader societal impacts of gene editing. Ensuring that advancements in CRISPR technology contribute equitably to public health will require transparency, comprehensive oversight, and a commitment to addressing the needs of marginalized communities.
The Promise of Curing Sickle Cell Disease
One of the most significant promises of CRISPR technology lies in its potential to provide cures for genetic conditions such as sickle cell disease. This painful disorder affects approximately 100,000 individuals in the United States alone, leading to severe health complications. By employing CRISPR to alter somatic cells, researchers have been able to reverse the genetic mutations that cause sickle cell disease, offering hope to many families who have endured the consequences of this condition. The prospect of a functional cure brings forth an optimistic outlook for patients and medical professionals alike.
Despite the potential benefits of curing sickle cell disease, ethical questions arise about the implications and accessibility of such treatments. The high cost associated with gene modification therapies leads to disparities within healthcare, creating challenges regarding who has the right to receive potentially life-saving procedures. Moreover, the ethical dilemma intensifies when considering the extent to which parents or guardians should exert influence over genetic traits for their children. While the promise of CRISPR technology to eradicate diseases is compelling, it is essential to engage in continuous dialogue surrounding equity and ethics in healthcare solutions.
The Role of Biomedical Ethics in Gene Editing
Biomedical ethics plays a crucial role in navigating the complexities of gene editing, especially as technologies like CRISPR become more prevalent in the medical field. Discussions surrounding gene editing often invoke questions related to consent, the role of parents and guardians, and the implications of altering genetic traits. With advancements allowing for modifications on both somatic and germline levels, there is a pressing need for a robust ethical framework to guide research and clinical applications. Ensuring that patients and families are adequately informed about the ramifications of gene editing is paramount.
Furthermore, the principles of biomedical ethics—beneficence, non-maleficence, autonomy, and justice—serve as a compass to navigate the challenges associated with gene editing. As researchers and clinicians grapple with the application of CRISPR technology, they must consider not only the medical outcomes but also the broader social impacts of their work. This commitment to ethical responsibility will be essential in fostering public trust, promoting health equity, and ensuring that the benefits of gene editing technologies are distributed fairly among all populations.
Risks and Unintended Consequences of Gene Editing
While CRISPR technology has opened new avenues for genetic interventions, it is essential to recognize the potential risks and unintended consequences that may accompany gene editing. As illustrated by Neal Baer’s discussion, the modification of genes can lead to unforeseen outcomes due to the complex interactions of genetic components within the body. For example, editing a single gene intended to lower LDL cholesterol may inadvertently affect other biological processes, highlighting the intricate nature of human genetics and the need for comprehensive research before widespread applications are made.
In addition to biological risks, gene editing generates concerns regarding ethical governance. The absence of universal regulatory standards grants rooms for potential abuses, especially in countries with less stringent oversight. Speculative scenarios, such as genetic enhancements for military purposes or designer babies, provoke important ethical questions surrounding the implications of manipulating human genetics. As society navigates the exhilarating possibilities of CRISPR technology, it is crucial to maintain a vigilant approach toward understanding both its potential benefits and risks.
The Debate Over Genetic Modification of Traits
The possibility of using CRISPR technology to modify traits presents a moral quandary that extends beyond mere medical necessity. As Baer mentions, ethical dilemmas arise when considering whether it is appropriate to edit genes associated with conditions that are not life-threatening, such as Down syndrome. This raises poignant questions: who gets to determine which traits are desirable or undesirable? Allowing parents or society at large to dictate genetic attributes could lead to increased social pressure and stigmatization of those who do not conform to certain standards. Such considerations warrant thorough ethical deliberation.
Moreover, the notion of modifying non-pathological traits could pave the way for a culture that values certain characteristics over others, heightening societal divisions. As gene editing technology progresses, discussions must shift to include not only the technical abilities of such advancements but also the moral implications and potential societal repercussions. Encouraging responsible discourse around gene editing is essential for shaping a future that values diversity and human variation rather than one that seeks uniformity through genetic alteration.
Oversight and Regulation of Gene Editing
The question of oversight in gene editing practices, particularly with technologies like CRISPR, is increasingly pertinent as the field rapidly evolves. Baer’s remarks about the challenges in monitoring international research practices shine a light on a critical oversight gap. For example, while certain countries have robust frameworks to regulate gene editing, others may lack stringent guidelines, allowing for risky experimentation without proper checks. The international community must collaborate to establish comprehensive regulatory frameworks that ensure the safety and ethical application of gene editing technologies across borders.
Moreover, effective oversight is not limited to monitoring research and clinical applications but also extends to public education and engagement. Informing the public about the risks and benefits of gene editing is crucial for fostering informed consent and promoting responsible use of technology. By creating open channels of communication between scientists, ethicists, and the public, we can work toward establishing a shared understanding of gene editing’s potential and pitfalls. This collaborative approach will help ensure that advancements in CRISPR technology are realized responsibly and ethically, benefiting all segments of society.
Cultural Perspectives on Genetic Variation
Cultural perspectives on genetic variation play a significant role in shaping societal attitudes toward gene editing technologies like CRISPR. As indicated in Baer’s discussion, the perceptions surrounding conditions like deafness or albinism as aspects of human diversity rather than pathology challenge the notion of ‘fixing’ genetic traits. Advocates from various cultural backgrounds emphasize the importance of recognizing the value of differences, which should lead to a broader understanding of genetic diversity as an enriching facet of the human experience rather than a defect needing correction.
These cultural perspectives underscore the necessity of inclusive dialogue when addressing the implications of gene editing. As society grapples with the advancements brought forth by CRISPR technology, it is vital to incorporate diverse voices and champion the need for respect toward all forms of human variation. Through this lens, gene editing can be approached not just as a medical tool for enhancement, but as a means to engage in deeper conversations about identity, belonging, and the ethical limits of human intervention in the natural world.
Future Directions in Gene Editing Research
The future of gene editing research will hinge on both technological advancements and the ethical frameworks developed to guide them. As scientists continue to refine CRISPR technology, exploring its applications across various fields—from agriculture to medicine—the potential for groundbreaking discoveries is vast. However, the directions taken in this research must include a thorough consideration of the associated ethical implications, especially with regard to health equity and access to these scientific innovations.
Additionally, interdisciplinary collaboration among researchers, ethicists, and community stakeholders will be essential for paving a responsible path forward in gene editing. Engaging diverse perspectives ensures that advancements in CRISPR technology serve the greater good and do not exacerbate existing social inequalities. As we look toward the future of gene editing, the ultimate goal should be to harness this powerful technology in a manner that is ethical, equitable, and beneficial to all members of society.
Frequently Asked Questions
What is CRISPR technology and how does it relate to gene editing?
CRISPR technology is a revolutionary gene editing tool that allows scientists to precisely alter DNA sequences within living organisms. It utilizes a natural defense mechanism found in bacteria, enabling targeted modification of genes, which has vast implications for medical research, including the potential treatment of genetic disorders and diseases.
What are the ethical concerns surrounding CRISPR technology in gene editing?
The ethics of gene editing with CRISPR technology raise significant questions about the implications of altering human DNA. Ethical concerns include the right to make decisions about genetic modifications, potential discriminatory practices against certain genetic traits, and the responsibilities of scientists in ensuring fair access to gene editing treatments.
How can CRISPR technology potentially cure sickle cell disease?
CRISPR technology has the capability to edit somatic cells to correct the genetic mutations causing sickle cell disease. By precisely targeting and modifying the defective genes in patients, scientists can provide a potential cure, allowing individuals to recover from the painful symptoms associated with this genetic disorder.
What is the relationship between health equity and CRISPR gene editing?
Health equity is a critical consideration in the context of CRISPR gene editing, as access to these innovative treatments may exacerbate existing healthcare disparities. The high costs associated with gene therapies can limit availability for marginalized populations, raising ethical concerns about who benefits from advancements in biomedical technologies.
What are the potential unintended consequences of CRISPR gene editing?
While CRISPR gene editing presents formidable possibilities, it can also lead to unintended consequences due to the complex interactions within the genome. Altering one gene may inadvertently affect other genes, leading to unforeseen health issues or mutations that could have lasting effects, highlighting the need for careful oversight and ethical consideration in its applications.
Who should make decisions about gene editing in humans using CRISPR technology?
Decisions about CRISPR-based gene editing in humans should involve a multidisciplinary approach that includes ethicists, scientists, policymakers, and public input. The complexity of gene modifications necessitates a careful balance of scientific knowledge and public ethical standards to determine what is acceptable and beneficial for society.
What role does oversight play in the use of CRISPR gene editing technologies?
Oversight is crucial in the use of CRISPR gene editing technologies to ensure ethical practices and prevent misuse. Regulatory bodies must establish guidelines for research, clinical applications, and modifications to human germline cells, ensuring that the benefits of gene editing are achieved responsibly while minimizing harm and ethical breaches.
| Key Point | Details |
|---|---|
| Ethical Dilemma | The central question posed is about the ethical implications of changing human differences through CRISPR. |
| Potential Cures | CRISPR may offer cures for diseases like sickle cell anemia, raising questions about the morality of such interventions. |
| Costs and Access | Curing sickle cell can cost around $2.2 million, raising issues of health equity and access. |
| Social Implications | What if parents choose genetic modifications based on personal preference? This opens discussions about parental rights versus child autonomy. |
| Oversight and Regulation | Concerns exist regarding who regulates gene editing and potential for misuse in countries with less oversight. |
| Unintended Consequences | Gene editing could lead to unforeseen health issues due to the complex nature of genetic interactions. |
Summary
CRISPR technology is revolutionizing the field of medicine by offering potential cures for genetic diseases, but it also raises significant ethical questions. As scientists explore the possibilities offered by CRISPR, it is essential to navigate the moral landscape carefully, ensuring that such advancements do not exacerbate inequalities or lead to unintended consequences. Balancing the benefits of curing illnesses like sickle cell disease with the ethical implications of genetic modifications is critical for the responsible use of this powerful technology.
Smoking Cessation for Teens: Varenicline Study Reveals Success
Smoking cessation for teens is a pressing public health issue as vaping becomes increasingly prevalent among young people. Innovative treatments, such as the FDA-approved varenicline, have emerged as promising options, significantly increasing the chances of quitting among teens. In recent clinical trials, researchers found that young adults taking varenicline had over three times the success rate of those relying solely on behavioral counseling, emphasizing the need for effective strategies to combat nicotine addiction. With vaping posing serious health risks, including addiction and exposure to harmful substances, it’s crucial that we support adolescents in quitting. By leveraging tools like varenicline, we can empower our youth to take bold steps towards healthier futures.
Adolescent nicotine addiction continues to surge, making it vital to explore alternative approaches to help young individuals break free from harmful habits. The challenge of quitting vaping necessitates effective mechanisms that resonate with the youth, particularly as many alternatives are geared towards an adult demographic. Various smoking cessation methods and aides, including prescription medications and behavioral support, are now being investigated for their efficacy on a younger audience. Given the alarming rise in vaping among teenagers, tailored solutions focusing on this demographic are essential to mitigate the associated health risks. With ongoing research and innovative treatment options, we are closer than ever to offering young people the support they need to quit vaping.
Understanding Vaping Cessation for Teens
Vaping among teens has surged over the past few years, presenting significant health risks. Understanding why adolescents become addicted to nicotine through vaping is crucial in shaping effective cessation strategies. Research indicates that teenage brains are still developing, making them particularly susceptible to nicotine addiction. Their preference for vaping over traditional smoking may be partly due to vapes being easier to use and less detectable, which increases the likelihood of experimentation. As vaping continues to rise among this age group, it’s essential that health professionals address these unique challenges through targeted interventions.
Teens often face peer pressure that makes quitting vaping more difficult, which is why comprehensive cessation programs are essential. These programs should include not only behavioral counseling but also FDA-approved aids like varenicline that demonstrate effectiveness in this demographic. By making resources accessible and providing education on the health risks of vaping, we can empower teenagers to make informed decisions that promote their health and well-being.
The Role of Varenicline in Quitting Vaping
Varenicline, an FDA-approved medication for smoking cessation, has shown promising results in helping young adults and teens quit vaping. In recent studies, participants who received varenicline were more than three times likely to successfully stop using vapes compared to those who received placebo treatments. This significant difference highlights the importance of pharmacological support in conjunction with behavioral therapy. Varenicline works by targeting nicotine receptors in the brain to reduce cravings and withdrawal symptoms, making the quitting process less daunting.
Moreover, what sets varenicline apart is its safety profile, particularly in younger populations. During clinical trials, no instances of participants who quit vaping transitioning to cigarettes were reported, underscoring its effectiveness without promoting alternative tobacco uses. By prescribing varenicline to adolescents aged 16 to 25, healthcare providers can facilitate healthier choices and potentially curb the growing trend of vaping-related health issues among young people.
FDA-Approved Smoking Aids and Their Impact
The introduction of FDA-approved smoking cessation aids marks a significant advancement in public health initiatives aimed at combating nicotine addiction. These medications, including varenicline, have undergone rigorous testing to ensure their safety and efficacy in helping individuals quit smoking and vaping. Their availability provides a new layer of support for teenagers who struggle with vaping addiction, enhancing the efficacy of treatment programs that already incorporate behavioral counseling.
Utilizing FDA-approved aids enables healthcare providers to offer a multifaceted approach to smoking cessation, particularly for youth. With a scientific basis for their use, these medications are crucial in a landscape where traditional methods may fall short. As vaping becomes increasingly normalized among teens, these smoking cessation aids offer essential strategies for reducing nicotine dependency and promoting healthier lifestyles.
Health Risks Associated with Vaping in Adolescents
The health risks associated with vaping among adolescents cannot be overstated. Vaping exposes young users to nicotine, which can derange neurodevelopment and potentially lead to long-term addiction. Furthermore, studies reveal that vapes may contain harmful substances, such as heavy metals and carcinogens, which are known to contribute to respiratory issues and other health complications. These risks highlight the urgent need for early intervention and cessation support tailored specifically for adolescents.
Additionally, the pervasive myth that vaping is a ‘safer’ alternative to smoking can lead to complacency among teenagers regarding their health. As education about the health risks of vaping increases, it’s crucial to communicate these dangers clearly to teens. Awareness campaigns coupled with effective cessation strategies will help dismantle the misconceptions surrounding vaping and encourage youths to opt for healthier choices.
Behavioral Counseling and its Importance in Cessation Treatments
Behavioral counseling plays a pivotal role in smoking cessation treatments, particularly for teenagers. The psychological aspects of addiction are complex, and addressing them requires more than just pharmacological interventions. Comprehensive counseling provides teens with tools to cope with cravings, urges, and emotional triggers that may lead them back to vaping. By integrating these behavioral strategies with medications like varenicline, we can enhance the likelihood of long-term success in quitting.
Moreover, counseling offers a supportive environment where teens can share their experiences and challenges with cessation. It fosters peer support and builds resilience, which are crucial during such a critical period in their lives. With increased access to behavioral counseling services, we can create a robust support system for young individuals battling nicotine addiction, leading to healthier lifestyles and reduced smoking rates in the future.
The Need for Further Research on Youth Vaping
Despite the promising results from recent studies on vaping cessation in teenagers, there remains a significant need for further research. Understanding the nuances of vaping culture among youth, including the social and environmental factors that contribute to vaping behavior, is essential. Ongoing studies can help identify the most effective treatment modalities for an even younger demographic, ensuring we address the root causes of nicotine addiction early.
Exploring additional therapeutic approaches alongside varenicline could yield new insights into effective smoking cessation methods. As vaping products evolve, so must our strategies for prevention and treatment. Continued research will inform best practices for health providers and policymakers, ultimately leading to better health outcomes for adolescents grappling with nicotine addiction.
Educating Teens About Vaping Risks
Educating teens about the health risks associated with vaping is a crucial first step in cessation efforts. Comprehensive education initiatives should focus on the immediate and long-term health consequences of vaping, emphasizing that substances in e-cigarettes can lead to serious respiratory and cardiovascular issues. Knowledge empowers teens to make informed decisions about their health, increasing the likelihood of quitting.
Moreover, schools and community organizations should collaborate to create engaging educational programs that resonate with teenagers. Utilizing social media platforms and interactive workshops can better capture their attention and foster a culture of health awareness. By investing in educational resources, we can lay the groundwork for a more informed generation that prioritizes health over misconceptions perpetuated by viral trends.
Community Support in Vaping Cessation
Community support plays an essential role in the success of vaping cessation efforts among teens. Establishing local support groups and activities focused on raising awareness about the health risks of vaping can foster a positive environment for those wanting to quit. Support from peers, family, and community leaders can provide the encouragement necessary for young people to seek help when they encounter challenges during their cessation journey.
Additionally, community-based initiatives can bridge the gap between healthcare providers and teens. By creating partnerships with schools, youth organizations, and healthcare facilities, we can enhance access to resources such as counseling and FDA-approved aids. Combining community outreach with effective smoking cessation programs can significantly improve quitting rates among adolescents, leading to healthier, nicotine-free futures.
Navigating Vaping Policies in Schools
As vaping becomes increasingly prevalent, schools must navigate policies that address vaping among students. Implementing clear anti-vaping policies can help deter use on campuses and promote a culture of wellness. Effective enforcement of these policies, coupled with education regarding the health risks of vaping, can create an environment that discourages nicotine use among teenagers.
Moreover, schools should consider integrating vaping prevention into their curricula. Teaching students about the dangers of vaping and the resources available for quitting, such as behavioral counseling and medications like varenicline, can empower them to make healthier choices. By fostering an atmosphere of support, schools play a critical role in reducing vaping rates and encouraging cessation among students.
Future Directions in Vaping Research and Treatment
Looking ahead, the landscape of vaping and nicotine addiction requires ongoing research to identify effective treatment options, especially for adolescents. Researchers must focus on developing age-appropriate cessation methods that consider the particular challenges faced by teens, such as peer influences and social media impacts. Innovative approaches may include digital therapeutics that leverage technology to provide continuous support, as well as community programs tailored to engage young users.
Additionally, further studies evaluating the long-term impacts of early nicotine exposure on brain development are critical. Understanding these effects will assist in shaping preventive strategies and treatment protocols. By prioritizing research in these areas, we can ensure that effective support systems are in place to combat the rising trend of vaping among teens, ultimately fostering healthier generations ahead.
Frequently Asked Questions
What is the best method for smoking cessation for teens who vape?
According to recent studies, the best method for smoking cessation for teens who vape is the use of varenicline, an FDA-approved medication that has been shown to effectively help young adults and teens quit vaping. Participants using varenicline had a success rate three times higher than those receiving only behavioral counseling.
How effective is varenicline for young adults looking to quit vaping?
Varenicline is highly effective for young adults looking to quit vaping. Clinical trials demonstrated that 51% of teens and young adults taking varenicline stopped vaping after 12 weeks, significantly outperforming the placebo group’s 14% success rate.
What are the health risks of vaping that teens should know about?
Teens should be aware of several health risks of vaping, including nicotine addiction, exposure to carcinogens, heavy metals, and pulmonary inflammation. Early exposure to nicotine through vaping can also increase the likelihood of future addiction to other substances.
Can FDA-approved smoking aids help teens quit vaping?
Yes, FDA-approved smoking aids like varenicline can help teens quit vaping. These medications have shown promising results in clinical trials, providing a safer and more effective option for youth struggling with nicotine addiction.
What support is available for teens attempting to quit vaping?
Teens attempting to quit vaping have access to various forms of support, including behavioral counseling and smartphone text support services like “This is Quitting”. Research shows that combining these resources with medications like varenicline can enhance the chances of quitting.
Are there any risks associated with using varenicline for smoking cessation in teens?
Varenicline has been found to be safe for teens aged 16 to 25. In clinical studies, no participants who quit vaping switched to smoking cigarettes, suggesting that varenicline can effectively aid in smoking cessation without leading to other nicotine sources.
How can teens access treatment for vaping cessation?
Teens aged 16 to 25 can access treatment for vaping cessation through healthcare providers who can prescribe varenicline, along with counseling and support services. It’s essential for teens to communicate their struggles with nicotine use to obtain effective treatment options.
| Key Points |
|---|
| FDA-approved varenicline proven effective for teens (16-25) quitting vaping. |
| Clinical trial results show varenicline users had three times higher quitting success than those with placebo (51% vs 14% at 12 weeks). |
| Participants engaged in behavioral counseling, but medication significantly enhanced success. |
| Vaping is prevalent among teens with health risks including nicotine addiction and potential future substance abuse. |
| No participants who quit vaping switched to cigarettes, indicating safety of varenicline in this group. |
Summary
Smoking cessation for teens is crucial as it helps them escape the cycle of nicotine addiction that begins with vaping. The recent study highlighting the effectiveness of varenicline presents a promising avenue for helping teens and young adults successfully quit vaping. With a threefold increase in quitting success compared to traditional methods, this FDA-approved medication alongside behavioral support offers a safe and effective strategy for addressing smoking cessation in this vulnerable population.